Concept 39.2: Innate Defenses Are Nonspecific
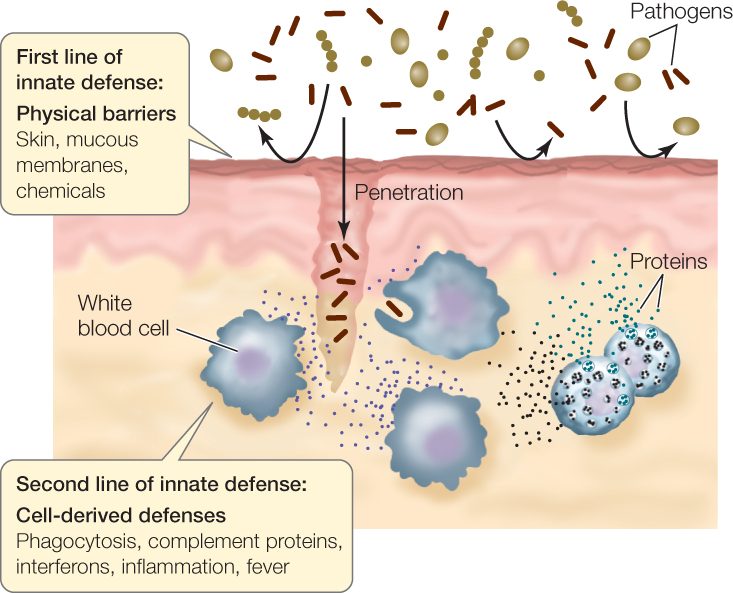
Innate, nonspecific defenses are general protection mechanisms that attempt to either stop pathogens from invading the body or quickly eliminate pathogens that do manage to invade. They are genetically programmed (innate) and “ready to go,” in contrast to adaptive, specific defenses, which take time to develop after a pathogen or toxin has been recognized as nonself. In mammals, innate defenses include physical barriers as well as cellular and chemical defenses (FIGURE 39.3).

Go to MEDIA CLIP 39.1 The Chase Is On: Phagocyte versus Bacteria
PoL2e.com/mc39.1
Barriers and local agents defend the body against invaders
The first line of innate defense is encountered by a potential pathogen as soon as it lands on the surface of the animal. Consider a pathogenic bacterium that lands on human skin. The challenges (physical, chemical, and biological) faced by the bacterium just to invade the body are formidable:
- The physical barrier of the skin: Bacteria rarely penetrate intact skin (which explains why broken skin increases the risk of infection).
- The saltiness of the skin: This condition is usually not hospitable to the growth of the bacterium.
- The presence of normal flora: Bacteria and fungi that normally live in great numbers on body surfaces without causing disease will compete with potential pathogens for space and nutrients.
If a pathogen lands inside the nose or another internal organ, it faces other innate defenses:
- Mucus is a slippery secretion produced by mucous membranes, which line various body cavities that are exposed to the external environment. Mucus traps microorganisms so they can be removed by the beating of cilia (see Concept 4.4), which continuously move the mucus and its trapped debris toward the outside of the body.
- Lysozyme, an enzyme made by mucous membranes, cleaves bonds in the cell walls of many bacteria, causing them to lyse (burst open).
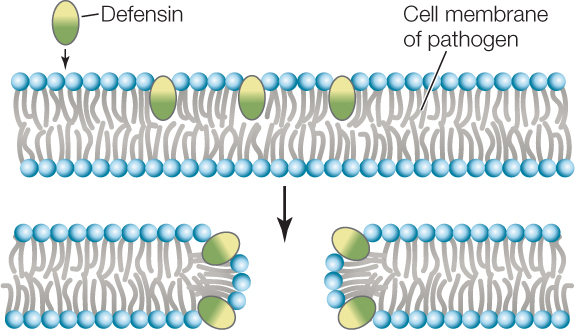
- Defensins, also made by mucous membranes, are peptides of 18–45 amino acids. They contain hydrophobic domains and are toxic to a wide range of pathogens, including bacteria, microbial eukaryotes, and enveloped (membraneenclosed) viruses. Defensins insert themselves into the cell membranes of these organisms and make the membranes freely permeable to water and all solutes, thus killing the invaders:Defensins are also produced inside phagocytes, where they kill pathogens trapped by phagocytosis. Plants also produce molecules that kill pathogens (see Concept 28.1).
- Harsh conditions in the internal environment can kill pathogens. For example, the gastric juice in the stomach is a deadly environment for many bacteria because of the hydrochloric acid and proteases that are secreted into it.
813
Cell signaling pathways stimulate additional innate defenses
Pathogens that are able to penetrate the body’s outer and inner surfaces encounter a second line of innate defenses. These include the activation of defensive cells. In some animals and plants, this activation involves recognition of nonself molecules by a class of receptors called pattern recognition receptors (PRRs). In mammals, these receptors are mainly present on phagocytes and natural killer cells. The Toll-like receptor shown in Figure 39.1 is an example. The molecules recognized by PRRs are called pathogen associated molecular patterns (PAMPs). These are molecules that are unique to large classes of microbes, such as bacterial flagellin and fungal chitin. Other well-known PAMPs include bacterial lipopolysaccharide, found in bacterial cell membranes, and nucleic acid variants that are unique to viruses, such as double-stranded RNA. Binding of PAMPs to PRRs stimulates signal transduction pathways that lead to a variety of responses. One response is the production of antimicrobial peptides such as defensins (see above). Other responses include phagocytosis of invading organisms, activation of natural killer cells, activation of the complement system, and production of cytokines.
Phagocytosis
Pathogenic cells, viruses, and virus-infected cells can be recognized by phagocytes, which then ingest the invaders by phagocytosis:
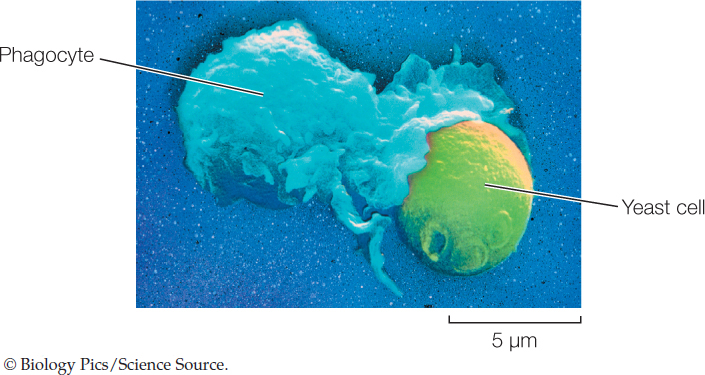
Once inside the phagocyte, the invader is killed either by hydrolysis within the lysosomes (see Figure 4.9) or by defensins.
Natural Killer Cells
One class of lymphocytes, known as natural killer cells, can distinguish between healthy body cells and those that are infected by viruses or have become cancerous. In the latter cases they initiate apoptosis (programmed cell death; see Concept 7.5) in the target cells. In addition to this nonspecific action, natural killer cells interact with the adaptive defense mechanisms by lysing target cells that have been tagged with antibodies.
Complement Proteins
Vertebrate blood contains more than 20 different proteins that make up the antimicrobial complement system. Once this system has been activated, the proteins function in a characteristic sequence, or cascade, with each protein activating the next:
- One complement protein binds to components on the surface of an invading cell. This binding helps phagocytes recognize and destroy the invading cell.
- Another protein activates the inflammation response (see below) and attracts phagocytes to the site of infection.
- Finally, other proteins lyse the invading cell.
The complement system can be activated by various mechanisms, including the innate and adaptive immune systems. In the latter case, the complement cascade is initiated by the binding of a complement protein to an antibody bound to the surface of the invading cell.
Cytokines
Cytokines are signaling proteins that are released by many cell types. Cytokines that are produced in response to PRR activation include inflammatory cytokines (some interleukins and tumor necrosis factor; see below) and interferons, which help increase the resistance of neighboring cells to infection. Interferons are found in many vertebrates, and their production is induced by a variety of molecules. One such inducer is double-stranded viral RNA; thus interferons are particularly important in defense against viruses. Interferons bind to receptors on the cell membranes of uninfected cells, stimulating a signaling pathway that inhibits viral reproduction if the cells are subsequently infected. In addition, interferons stimulate the cells to hydrolyze bacterial or viral proteins to peptides, an initial step in adaptive immunity.
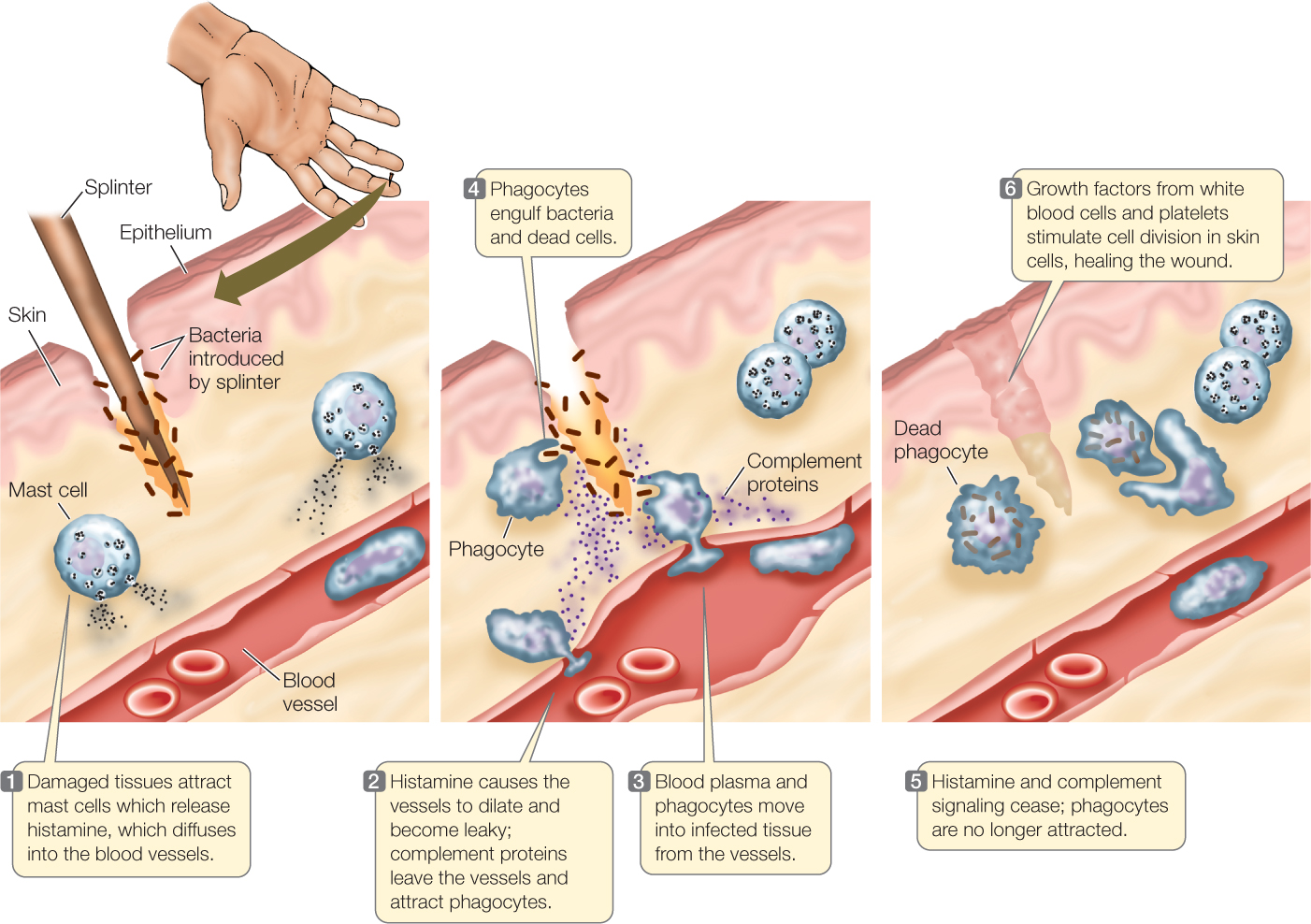
Inflammation is a coordinated response to infection or injury
When a tissue is damaged because of infection or injury, the body responds with inflammation: redness, swelling, and heat near the damaged site, which can then become painful. This response can happen almost anywhere in the body, internally as well as on the outer surface. Inflammation is an important phenomenon: it isolates the area to stop the spread of the damage; it recruits cells and molecules to the damaged location to kill any pathogens that might be present; and it promotes healing.
Among the first responders to tissue damage are mast cells, which adhere to the skin and the linings of organs and release numerous chemical signals, including:
- Tumor necrosis factor, a cytokine protein that kills target cells and activates immune cells
- Prostaglandins, fatty acid derivatives that play roles in various responses, including the initiation of inflammation in nearby tissues
- Histamine, an amino acid derivative that increases the permeability of blood vessels to white blood cells and molecules so they can act in nearby tissues
The redness and heat of inflammation result from the dilation of blood vessels in the infected or injured area (FIGURE 39.4). Phagocytes enter the inflamed area, where they engulf pathogens and dead tissue cells. Phagocytes are responsible for most of the healing associated with inflammation. They produce several cytokines, which (among other functions) can signal the brain to produce a fever. This rise in body temperature accelerates lymphocyte production and phagocytosis, thereby speeding the immune response. In some cases pathogens are temperature-sensitive, and their growth is inhibited by the fever. The pain of inflammation results from increased pressure due to swelling, the action of leaked enzymes on nerve endings, and the action of prostaglandins, which increase the sensitivity of the nerve endings to pain. (Recall that in Chapter 3 we described aspirin and how it alleviates pain by blocking the synthesis of prostaglandins.)
814
Go to ACTIVITY 39.1 Inflammation Response
PoL2e.com/ac39.1
Following inflammation, pus may accumulate. Pus is a mixture of leaked fluid and dead cells: bacteria, white blood cells, and damaged body cells. Pus is a normal result of inflammation, and is gradually consumed and further digested by macrophages. If there is a wound, platelets—small, irregularly shaped cell fragments that are present in the blood—aggregate at the wound site. The platelets produce growth factors that stimulate nearby skin cells to divide and heal the wound.
Inflammation can cause medical problems
Although inflammation is generally a good thing, sometimes the inflammatory response is inappropriately strong:
- In an allergic reaction, a nonself molecule that is normally harmless binds to mast cells, causing the release of histamine and subsequent inflammation (along with itchy, watery eyes, and rashes in some cases). The nonself molecule may come from food or from the environment—for example, from the surface of a plant pollen grain (as in hay fever) or a particle in dust.
- In autoimmune diseases such as rheumatoid arthritis, the immune system fails to distinguish between self and nonself, and attacks tissues in the organism’s own body. In these cases the inflammation can be local, attacking an organ, or general, affecting tissues throughout the body.
- In sepsis, the inflammation that is due to a bacterial infection does not remain local. Instead it becomes widespread, with the dilation of blood vessels throughout the body. The resulting drop in blood pressure is a medical emergency and can be lethal.
CHECKpoint CONCEPT 39.2
- Outline the sequence of innate defenses encountered by a pathogenic bacterial cell if it is ingested in food.
- Antihistamines are used to treat the symptoms, such as sneezing, that are due to inflammation caused by irritants in the airways. How do you think antihistamines might work?
- A massive inflammation caused by a food allergy can be treated with an injection of epinephrine. Refer to the description of epinephrine’s effects in Concept 35.2. How do you think this hormone relieves the inflammation symptoms?
815
In most instances innate immunity is sufficient to block a pathogen from affecting the body. But many pathogens are present in huge numbers (think of a viral infection), and some may escape the innate defenses and begin to proliferate in the body. In these cases, adaptive immunity takes over.