14.1 INTRODUCTION: Understanding Psychological Disorders
KEY THEME
Understanding psychological disorders includes considerations of their origins, symptoms, and development, as well as how behavior relates to cultural and social norms.
KEY QUESTIONS
What is a psychological disorder, and what differentiates abnormal behavior from normal behavior?
What is DSM-5, and how was it developed?
How prevalent are psychological disorders?
Does the cartoon make you smile? The cartoon is humorous, but it’s actually intended to make some serious points. It reflects several common misconceptions about psychological disorders that we hope to dispel in this chapter.
First, there’s the belief that “crazy” behavior is very different from “normal” behavior. Granted, sometimes it is, like Elyn’s bizarre pronouncements from the roof in front of her classmates. But as you’ll see throughout this chapter, the line that divides “normal” and “crazy” behavior is often not as sharply defined as most people think. In many instances, the difference between normal and abnormal behavior is a matter of degree. For example, as you leave your apartment or house, it’s normal to check or even double-check that the door is securely locked. However, if you feel compelled to go back and check the lock 50 times, it would be considered abnormal behavior.
The dividing line between normal and abnormal behavior is also often determined by the social or cultural context in which a particular behavior occurs. For example, among traditional Hindus in India, certain dietary restrictions are followed as part of the mourning process. It would be a serious breach of social norms if an Indian widow ate fish, meat, onions, garlic, or any other “hot” foods within six months of her husband’s death. A Catholic widow in the United States would consider such restrictions absurd.
Second, when we encounter people whose behavior strikes us as weird, unpredictable, or baffling, it’s easy to simply dismiss them as “crazy” as in the cartoon. Although convenient, such a response is too simplistic, not to mention unkind. It could also be wrong. Sometimes, unconventional people are labeled as crazy when they’re actually just creatively challenging the conventional wisdom with new ideas.
Even if a person’s behavior is seriously disturbed, labeling that person as “crazy” tells us nothing meaningful. What are the person’s specific symptoms? What might be the cause of the symptoms? How did they develop? How long can they be expected to last? And how might the person be helped? The area of psychology and medicine that focuses on these questions is called psychopathology—the scientific study of the origins, symptoms, and development of psychological disorders. In this chapter and the next, we’ll take a closer look at psychological disorders and their treatment.
psychopathology
The scientific study of the origins, symptoms, and development of psychological disorders.
Finally, there is still a strong social stigma attached to suffering from a psychological disorder (Ben-Zeev & others, 2010; Tucker & others, 2013). Because of the social stigma that can be associated with psychological disorders, people are often reluctant to seek the help of mental health professionals (Arboleda-Florez & Sartorius, 2008; Bathje & Pryor, 2011). People who are under the care of a mental health professional often hide the fact, telling only their closest friends—and understandably so. Being labeled “crazy” carries all kinds of implications, most of which reflect negative stereotypes about people with mental illness (Wirth & Bodenhausen, 2009). In the Critical Thinking box “Are People with a Mental Illness as Violent as the Media Portray Them?”, we discuss the accuracy of such stereotypes in more detail.
What Is a Psychological Disorder?
What exactly are we talking about when we say that someone has a psychological or mental disorder? A psychological disorder or mental disorder can be defined as a pattern of behavioral or psychological symptoms that causes significant personal distress, impairs the ability to function in one or more important areas of life, or both (DSM-5, 2013). An important qualification is that the pattern of behavioral or psychological symptoms must represent a serious departure from the prevailing social and cultural norms. Hence, the behavior of a traditional Hindu woman who refuses to eat onions, garlic, or other “hot” foods following the death of her husband is perfectly normal because that norm is part of the Hindu culture.
psychological disorder or mental disorder
A pattern of behavioral and psychological symptoms that causes significant personal distress, impairs the ability to function in one or more important areas of life, or both.
What determines whether a given pattern of symptoms or behaviors qualifies as a psychological disorder? Throughout this chapter, you’ll notice numerous references to DSM-5. DSM-5 stands for Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, which was published by the American Psychiatric Association in 2013.
DSM-5
Abbreviation for the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition; the book published by the American Psychiatric Association that describes the specific symptoms and diagnostic guidelines for different psychological disorders.
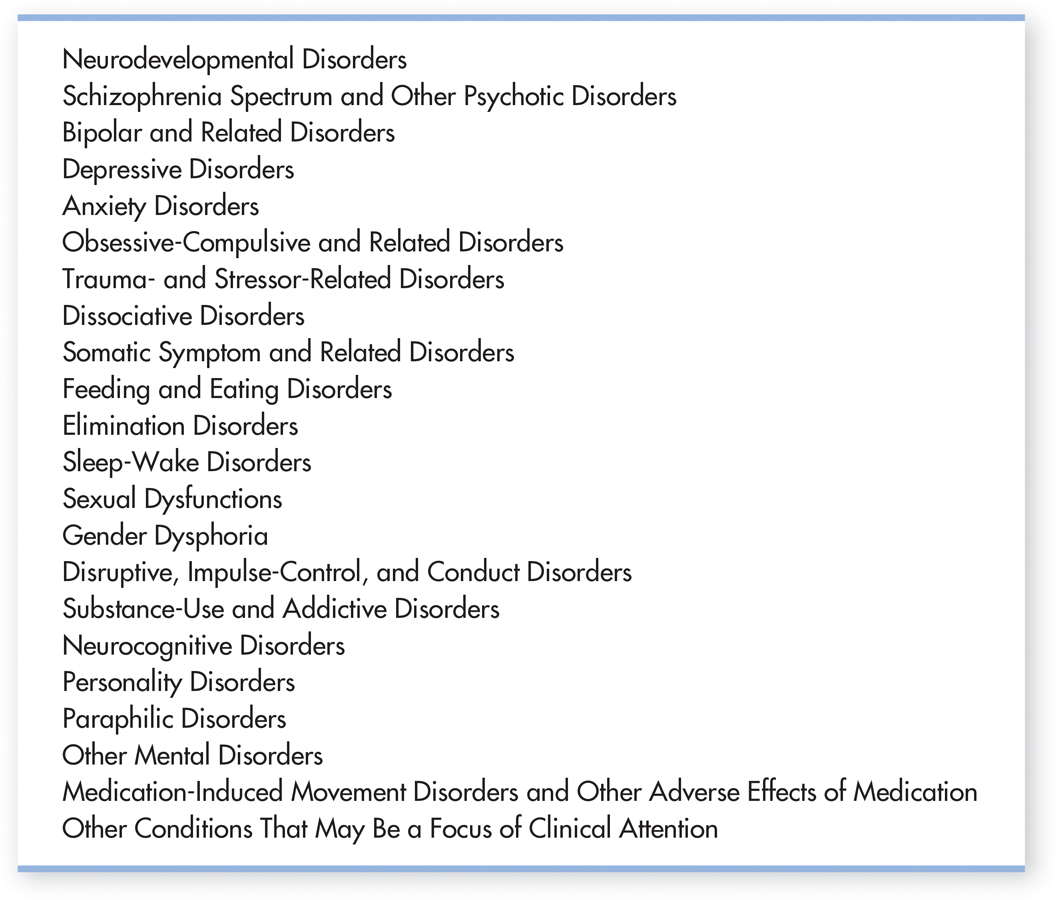
DSM-5 is a book that describes more than 260 specific psychological disorders, plus numerous additional conditions, like child physical abuse and educational problems. It provides codes for each disorder, and includes the symptoms, the criteria that must be met to make a diagnosis, and the frequency, typical course, and risk factors for each disorder. It also includes issues related to gender and culture for each disorder. A list of the major diagnostic classifications in DSM-5 is shown in FIGURE 14.1 below. DSM-5 provides mental health professionals with both a common language for labeling disorders and comprehensive guidelines for diagnosing them. DSM-5 also increasingly matches the disorders outlined in a similar manual utilized internationally, the World Health Organization’s International Classification of Diseases (ICD). (As of October 2014, mental health clinicians were expected to use codes from the ICD when seeking reimbursement through health insurance companies.)
CRITICAL THINKING
Are People with a Mental Illness as Violent as the Media Portray Them?
Are people with a psychological disorder more violent than other people? When a heinous crime occurs, such as a mass shooting in a public place, people tend to react by assuming that the perpetrator “must be crazy.” Such statements may reflect the belief that mental illness and violent crime are closely linked. As Mary Camp and her colleagues (2010) write, “those categorized as mad are expected to be violent, unpredictable, or antisocial.”
In some cases, such as the 2012 shootings in an elementary school in Newtown, Connecticut, or the 2014 shootings near the University of California, Santa Barbara, the killers do have symptoms of mental disturbance. Yet the vast majority of violent crimes, even heinous ones, are committed by people who are not mentally ill.
Multiple studies have found that people with a major mental illness belong to the most stigmatized group in modern society (Hinshaw & Stier, 2008; Schomerus & others, 2012). Substantial progress has been made in the understanding and treatment of psychological disorders. However, in much of the popular media, people with psychological disorders are still portrayed in highly negative, stereotyped ways (Klin & Lemish, 2008; Nairn & others, 2011). One stereotype is that of the mentally disturbed person as a helpless victim. The other stereotype is that of the mentally disordered person as an evil villain who is unpredictable, dangerous, and violent (Camps & others, 2010). For example, many of the criminals in the Batman series, including the Joker and the Riddler, end up imprisoned in the fictional Arkham Asylum for the Criminally Insane after they are captured (Daniels, 2008).
One comprehensive survey found that although 5 percent of “normal” television characters are murderers, 20 percent of “mentally ill” characters are killers (Gerbner, 1998). The same survey found that about 40 percent of “normal” characters were violent, but 70 percent of characters labeled as mentally ill were violent. This trend is also apparent in stories about real people. A study of Canadian news stories in 20 major newspapers over five years found that 40 percent of articles that discussed mental illness put it in the context of “danger, violence, or criminality” (Whitley & Berry, 2013). These media stereotypes reflect and reinforce the widespread belief among Americans that most people with mental illness are violent and threatening (Diefenbach & West, 2007).

This public perception that people with a mental illness are dangerous contributes to the stigma of mental illness (Fazel & others, 2009; Torrey, 2011). But let’s look at the evidence. Are people with mental disorders more violent than other people?
One groundbreaking study by psychologist Henry Steadman and his colleagues (1998) monitored the behavior of more than 1,000 former mental patients in the year after they were discharged from psychiatric facilities. For their control group, they also monitored a matched group of people who were not former mental patients but were living in the same neighborhood.
The researchers found that, overall, the former mental patients did not have a higher rate of violence than the comparison group. Former mental patients who demonstrated symptoms of substance use disorder were the most likely to engage in violent behavior. However, the same was also true of the control group. In other words, substance use disorder was associated with more violent behavior in all participants, whether they had a history of mental illness or not. The study also found that the violent behavior that did occur was most frequently aimed at friends and family members, not at strangers.
MYTH !lhtriangle! SCIENCE
Is it true that most people with a psychological disorder are violent?
Recent meta-analytic research reviews have confirmed the general finding that substance abuse greatly increases the risk of violent behavior by people who have been diagnosed with a severe mental illness, such as schizophrenia (see Douglas & others, 2009; Fazel & others, 2009). Beyond substance abuse, there is evidence that people with severe mental disorders who are experiencing extreme psychological symptoms, such as bizarre delusional ideas and hallucinated voices, do display a slightly higher level of violent and illegal behavior than do “normal” people (Bucci & others, 2013; Malla & Payne, 2005). However, the person with a mental disorder who is not suffering from such symptoms is no more likely than the average person to be involved in violent or illegal behavior. Other factors, such as a family history of violence, living in impoverished neighborhoods, and abusing drugs or alcohol, are stronger predictors of violence (Nederlof & others, 2013; Norko & Baranoski, 2005; Singh & others, 2012). It also is important to point out that people with some kinds of mental illness are a good deal more likely to be the victims of a violent crime than other people (Short & others, 2013).
Canadian psychologist Kevin Douglas and his colleagues (2009) emphasize that the overall size of the association between psychosis and violence is relatively small. As they point out, “Most violent individuals are not psychotic, and most psychotic individuals are not violent.”
Clearly, the incidence of violent behavior among current or former mental patients is exaggerated in media portrayals. In turn, the exaggerated fear of violence from people with a psychological disorder contributes to the stigma of mental illness (Fazel & others, 2009). As psychologists Stephen Hinshaw and Andrea Stier (2008) emphasize, “Media depictions that routinely and inevitably link all forms of mental disorder with physical violence are stereotypic and inaccurate. Indeed, empirical data reveal that people with mental illness are far more likely to be victims of violent crime than are other individuals, and far more likely to be victims than to be perpetrators of violence.”
CRITICAL THINKING QUESTIONS
Can you think of any reasons why people with psychological disorders are more likely to be depicted as villains than members of other social groups?
Can you think of any television shows or movies in which characters with a severe psychological disorder were shown in a sympathetic light? If so, are such depictions more or less common than depictions of people with a mental illness as dangerous or violent?
What evidence could you cite to challenge the notion that people with psychological disorders are dangerous?
The first edition of Diagnostic and Statistical Manual was published in 1952. With each new edition, the number of distinct disorders has progressively increased—from fewer than a hundred in the first edition to more than three times that number in recent editions, including DSM-5 (Frances & Widiger, 2012; Horwitz, 2002; Houts, 2002). Some disorders that are relatively well known today, such as eating disorders, attention-deficit/hyperactivity disorder, and social anxiety disorder, were not added until later editions. And, some behavior patterns that were categorized as “disorders” in early editions, such as homosexuality, have been dropped from later editions because they are no longer considered to be psychological disorders.
It’s important to understand that DSM-5 was not written by a single person or even a small group of experts. Rather, DSM-5 represents the consensus of hundreds of mental health professionals, mostly psychiatrists and clinical psychologists, representing many different organizations and perspectives. DSM-5 was developed over twelve years. Teams of mental health professionals conducted extensive reviews of the research findings for each category of mental disorder and conducted field trials, studies that examined how well the DSM worked in clinical settings. The APA also developed a Web site to allow both professionals and the public to provide feedback.
Despite these efforts, DSM-5 has many critics (see Frances, 2012; Frances & Widiger, 2012; Wakefield, 2013a; G. Watts, 2012). More specifically, it has been criticized for:
inclusion of some conditions that are too “normal” to be considered disorders, such as extreme sadness related to bereavement (Maj, 2012; Wakefield, 2013b; Watts, 2012)
use of arbitrary cutoffs to draw the line between people with and without a particular disorder (J. Cohen & others, 2011; Insel, 2013; Livesley, 2011)
gender bias (Marecek & Gavey, 2013; Yonkers & Clarke, 2011)
possible bias resulting from the financial ties of many DSM-5 authors to the pharmaceutical industry, which might benefit from the expansion of mental illness categories or loosening of criteria for diagnoses (Cosgrove & Krimsky, 2012)
Finally, many critics believe that DSM-5 blurs the distinction between everyday normal unhappiness and “mental illness” (Watts, 2012). If the threshold for diagnosing mental disorders is set too low, some critics argue, too many people will be diagnosed with a “mental disorder” (Angell, 2011; Frances, 2010).
Despite its flaws, DSM-5 is the most comprehensive and authoritative set of guidelines available for diagnosing psychological disorders. Thus, we’ll refer to the DSM often in this chapter.
Question 14.1
AGFczuRa/kJ83ahtosE5sdQsyibiiJcEG9GJEg34WGNsTYUvTtdvrp25zV5qLsX1ivL0wKe0Zb9vvqKVeMd2t5e7nCaxFfwrZ4wAiMe39Ks8O1/gvNFMv6KY30CDAmNaLJsZrSPL6S93hkoJ3WqowfrxrNobKerNYURNKGebn5iwV9Rx1vxCNfsrsHIDhroN8eRweJaSi+cffjNp8d+fWOhPyhuO9id3pPDRI4FpPf7S35A5Z7wGYgrWEWsWDXUrrSCNZQ==The Prevalence of Psychological Disorders: A 50–50 CHANCE?

Just how common are psychological disorders? To investigate that question, researcher Ronald C. Kessler and his colleagues (2005a, 2005b) conducted a nationally representative survey of more than 9,000 Americans, ages 18 and older. Called the National Comorbidity Survey Replication (NCS-R), the survey involved more than two years of face-to-face interviews throughout the country. Participants were asked if they had experienced specific symptoms of psychological disorders (1) during the previous 12 months and (2) at any point in their lives. They were also asked about possible risk factors associated with mental disorders, such as substance use.
The NCS-R results reconfirmed many of the findings of previous national surveys, including the finding that psychological disorders are much more prevalent than many people believe (Kessler & others, 2005c). Specifically, the NCS-R found that one out of four respondents (26 percent) reported experiencing the symptoms of a psychological disorder during the previous year (Kessler & others, 2005b). The NCS-R and other surveys like it also reveal a high degree of comorbidity, which means that people diagnosed with one disorder are also frequently diagnosed with another disorder as well.
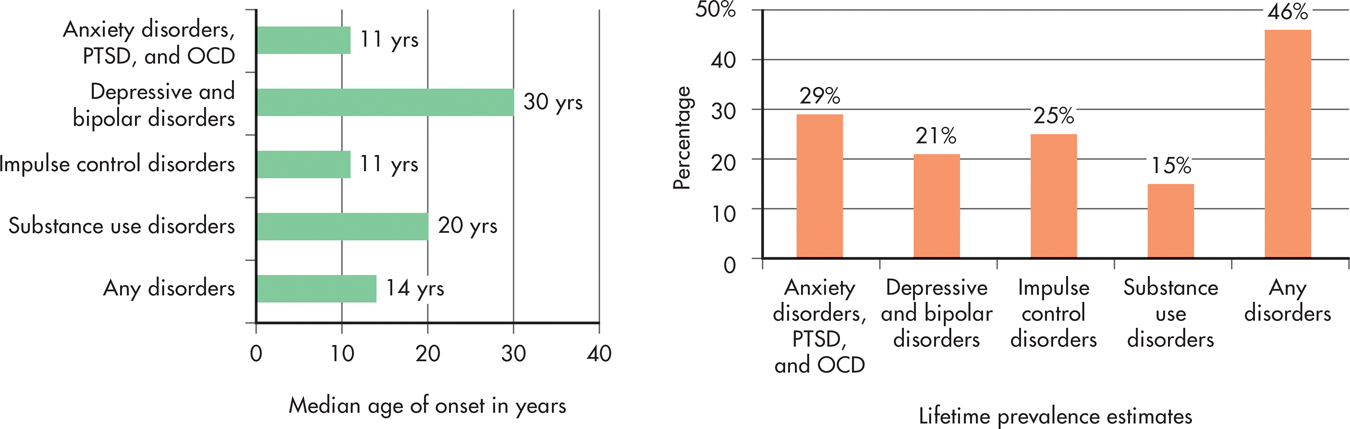
FIGURE 14.2 shows the typical age of onset for some of the common mental disorders reported by the NCS-R respondents at any point in their life. As you can see in the left-hand graph, the different categories of mental disorders vary significantly in the median age of onset. Anxiety disorders and impulse-control disorders tend to begin at a much earlier age—around age 11—as compared to substance abuse disorders or mood disorders. In the right-hand graph, you can see the lifetime prevalence of the same categories of mental disorders. Like the original National Comorbidity Survey, the NCS-R found that almost one out of two adults (46%) had experienced the symptoms of a psychological disorder at some point thus far in their lives.
The mentally ill are not some distinct set of “them” out there who are completely different from “us” sane people. Instead, the vast majority of us have been touched by some form of mental illness at some time in our lives either through personal experience or through the illness of a close loved one.
—Ronald C. Kessler (2003a)
Rates of mental illness are high not just in the United States, but globally. In a large-scale study conducted in conjunction with the World Health Organization, researchers surveyed about 85,000 people in 17 countries from almost every continent (Kessler & others, 2007). The lifetime rate of mental illness is about one third, with rates varying across countries—from about 12% in Nigeria to almost 50% in the United States (Wang & others, 2011). But estimates for countries with the lowest rates, like Nigeria, are likely to be biased because of a cultural stigma in disclosing symptoms of psychological disorders (Gureje & others, 2006).
MYTH !lhtriangle! SCIENCE
Is it true that psychological disorders are rare?
Although it might initially seem disturbing to think that one-third to one-half of the adult population in the United States will experience the symptoms of a mental disorder, lead researcher Ronald C. Kessler helps put these findings into perspective. As Kessler (2003b) points out,
It wouldn’t surprise anyone if I said that 99.9% of the population had been physically ill at some time in their life. Why, then, should it surprise anyone that 50% of the population has been mentally ill at some time in their life? The reason, of course, is that we invest the term “mentally ill” with excess meaning. A number of common mental illnesses, like adjustment disorders and brief episodes of depression, are usually mild and self-limiting. Many people experience these kinds of disorders at some time in their lives.
The NCS-R found that most people in the United States with the symptoms of a mental disorder (59 percent) received no treatment during the past year. Of those who did receive some kind of treatment, it was usually provided by a general medical practitioner, psychiatrist, or mental health specialist. Even so, the treatment provided was often inadequate, falling short of established treatment guidelines (Wang & others, 2005). These trends are shared globally. People in developing countries are even less likely than those in developed countries to seek treatment (Wang & others, 2011). In most countries, including the United States, mental health care is more likely to be provided by general medical practitioners than by any kind of mental health clinician (Wang & others, 2011).
Think Like a SCIENTIST
Tracking the incidence of mental health problems is challenging. Can internet searches reveal trends? Go to LaunchPad: Resources to Think Like a Scientist about Tracking Mental Illness Online.

It seems clear that many people who could benefit from mental health treatment don’t receive it. Several factors contribute to this unmet need, including lack of insurance, low income, and living in developing countries or rural areas of developed countries where mental health care facilities might not be available (Santiago & others, 2013; Wang & others, 2011). Some people lack awareness about psychological disorders or shun treatment for fear of being stigmatized for seeking help with troubling psychological symptoms.
On the other hand, it also seems clear that most people manage to weather psychological symptoms without becoming completely debilitated and needing professional intervention (Mojtabai & others, 2011). One explanation for this is that people use a variety of coping strategies—some more effective than others—to manage psychological symptoms.
But it’s important to remember that even ineffective strategies can appear to be effective. Why? Because the symptoms of many psychological disorders, especially those involving mild to moderate symptoms, diminish with the simple passage of time or with improvements in the person’s overall situation. Nevertheless, there are many effective treatments available for psychological disorders that can produce improvements that occur much more quickly and endure longer. We’ll look at the different types of therapies used to treat psychological disorders in the next chapter.
For the remainder of this chapter, we’ll focus on psychological disorders in six DSM-5 categories: anxiety, posttraumatic stress, and obsessive-compulsive disorders; depressive and bipolar disorders; eating disorders; personality disorders; dissociative disorders; and schizophrenia. Along with being some of the most common disorders encountered by mental health professionals, they’re also the ones that our students ask about most often. To help you distinguish between normal and maladaptive behaviors, we’ll start the discussion of each mental disorder category by describing behavior that falls within the normal range of psychological functioning, such as normal feelings of anxiety or normal variations in mood.
TABLE 14.1, describes other categories of mental disorders contained in the DSM-5. Some of these disorders have been discussed in previous chapters. In the Psych for Your Life section at the end of this chapter, we’ll look at what you can do to help prevent one of the most disturbing consequences of psychological problems—suicide.
Some Additional Diagnostic Categories in DSM-5
| Diagnostic Category | Core Features | Examples of Specific Disorders |
|---|---|---|
| Neurodevelopmental disorders | Includes a wide range of developmental, behavioral, learning, and communication disorders that are usually first diagnosed in infancy, childhood, or adolescence. Symptoms of a particular disorder may vary depending on a child’s age and development level. |
Autistic spectrum disorder: Onset of symptoms prior to age of 3. Characterized by (1) deficits in social communication and social interaction and (2) restricted, repetitive behaviors, interests, and activities; diagnosed according to level of symptom of severity, ranging from “requiring support” to “requiring very substantial support.” Tourette’s disorder: Onset prior to age of 18. Characterized by motor tics, such as recurring spasmodic movements of the head or arms, and vocal tics, such as recurring and sudden clicking, grunting, or snorting sounds. Sometimes involves uncontrollable utterances of profane or obscene words. |
| Substance-related and addictive disorders (see Chapter 4) | Characterized by a cluster of cognitive, behavioral, and physiological symptoms indicating that the individual continues using the substance or behavior despite significant problems related to the substance or behavior. |
Substance use disorder: Recurrent substance use that involves impaired control, disruption of social, occupational, and interpersonal functioning, and the development of craving, tolerance, and withdrawal symptoms. Gambling disorder: Persistent gambling that disrupts personal, family, and/or vocational pursuits. |
| Somatic symptom and related disorders | Characterized by persistent, recurring complaints of bodily (or somatic) symptoms that are accompanied by abnormal thoughts, feelings, and behaviors in response to these symptoms. |
Somatic symptom disorder: characterized by excessive worry or distress that is out of proportion to the seriousness of physical symptoms that are present. Illness anxiety disorder: excessive preoccupation with one’s health and worry about illness despite the absence of serious physical symptoms. |
| Paraphilic disorders (see Chapter 10) | Group of disorders involving intense and persistent sexual interest in inappropriate objects, activities, or people that causes distress or impairment to the person or distress or harm to others. |
Voyeuristic disorder: Recurrent and intense sexual arousal from observing a person who is undressing, naked, or engaging in sexual activity. Fetishistic disorder: Recurrent, intense, sexually arousing fantasies, urges, or behaviors, usually involving nonliving objects, such as female undergarments, shoes, boots, or other articles of clothing that causes significant personal distress or psychosocial role impairment. |
| Disruptive, impulse-control, and conduct disorders | Varied group of disorders involving problems in the self-control of emotions and behaviors and which are manifested in behaviors that harm or violate the rights of others. |
Kleptomania: The recurrent failure to resist impulses to steal items that are not needed for personal use or for their monetary value. Pyromania: Deliberately setting fires on more than one occasion, accompanied by pleasure, gratification, or relief of tension. |
| Source: American Psychiatric Association (2013). | ||
| This table includes some of the main diagnostic categories that are not covered in this chapter. We cover the major classes of psychological disorders in this chapter. Other important, but less common, diagnostic categories are shown here. | ||
Test your understanding of Understanding Psychological Disorders with
 .
.