16-1 Multidisciplinary Research on Brain and Behavioral Disorders
Chapter 7 surveys research methods ranging from single-
Brain research is multidisciplinary. One way to summarize methods of studying links between brain and behavior is to consider them from the macro level of the whole organism down to the molecular level of neuronal excitation and inhibition. Behavioral studies by their nature investigate the whole organism, but understanding the whole organism requires understanding its parts—
Section 3-3 reviews genetics, genetic engineering, and epigenetic mechanisms; Section 7-5 explores techniques for measuring genetic and epigenetic influences.
Molecular biology offers neuroscientists varied approaches to studying behavior. Scientists can breed strains of animals, such as fruit flies, fish, or mice, with either a gene knocked out (deleted or inactivated) or a gene inserted. Knockout technology is used both to create animal models of human disorders and to generate treatments for neurobehavioral disorders. Variations on this technology include methods for turning genes on or off for periods of time. What is clear from this research is that the genes related to disordered behavior in fruit flies, fish, and mice are largely the same as those related to similar disordered behavior in people.
Freud was limited to probing the brain with conversation. Today, brain imaging techniques allow behavioral neuroscientists to describe structures and pathways in an individual brain and the changes it undergoes during development, learning, and after damage, all without directly accessing the brain. Understanding the brain’s structure and function leads to understanding that individual brains differ—
Causes of Disordered Behavior
Neuroscientists presume that abnormal brain functioning results in disordered behavior. Evidence for brain abnormalities is relatively straightforward in neurological disorders, and at least in a general sense, the causes are largely known:
Focus 3-4 describes Huntington disease’s genetic basis; Focus 5-2, neural degeneration in Parkinson disease; Focus 2-3, symptoms and aftereffects of stroke; and Focus 4-2, myelin breakdown in MS.
Genetic errors, as in Huntington disease
Epigenetic mechanisms at work prenatally, later in life, even in succeeding generations
Progressive cell death resulting from neurodegenerative causes, as in Parkinson or Alzheimer disease
Rapid cell death, as in stroke or traumatic brain injury
Loss of neural function and connections seen in disorders such as multiple sclerosis and myasthenia gravis
565
In contrast to these organic neurological disorders, far less is known about neurobiological causes of behavioral and psychiatric disorders. But results of neurobiological studies of pathology and newer research methods are revealing clues to causation: changes in the brain’s structure or activity are implicated. Table 16-1 lists the most likely causal categories underlying behavioral disorders, micro to macro.
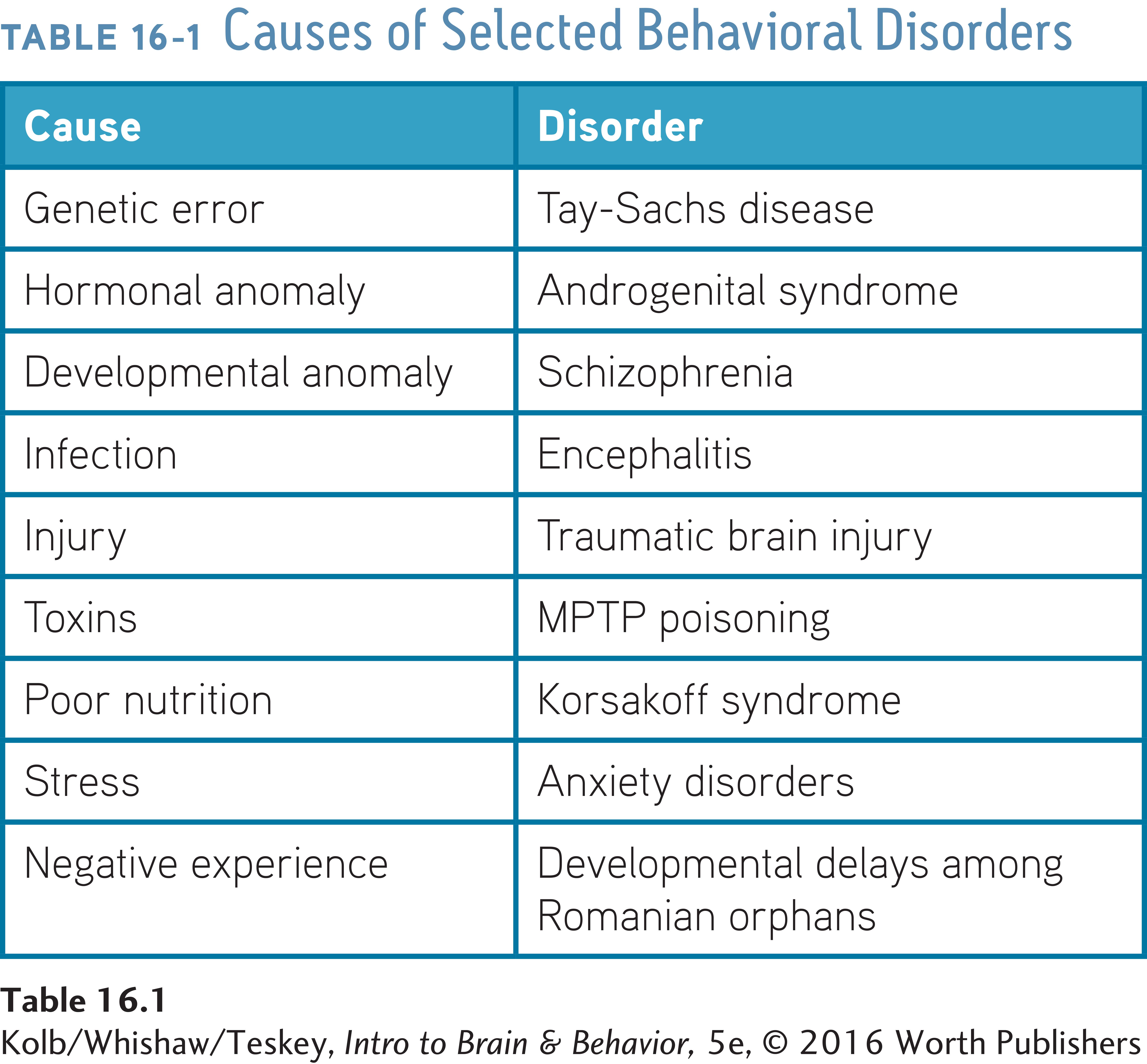
At the microscopic level is genetic error, such as that responsible for Tay-
Investigating the Neurobiology of Behavioral Disorders
A single brain abnormality can cause a behavioral disorder, explaining everything about it and its treatment. Phenylketonuria (PKU) is an example. PKU results from a defect in the gene for phenylalanine hydroxylase (PHA), an enzyme that breaks down the amino acid phenylalanine. Babies with PKU have elevated blood levels of phenylalanine, leading to intellectual impairments, seizures, and other physiological conditions. To inherit PKU, both parents must carry a defective PHA gene. This recessive condition confers resistance to certain fungal toxins. About 400 mutations of the PHA gene are known (Foroozani et al., 2015).
Left untreated, PKU causes severe intellectual disability, but PKU can be treated just by restricting dietary intake of phenylalanine—
If other behavioral disorders were as simple and well understood as PKU, neuroscience research could quickly yield cures for them. Many disorders do not result from a single genetic abnormality, however, and the causes of most disorders remain conjectural. The major problem: diagnosis of a disability is based mainly on behavioral symptoms, and behavioral symptoms give few clues to specific neurochemical or neurostructural causes.
This problem also appears in treating PKU. Table 16-2 lists what is known about PKU at different levels of analysis: genetic, biochemical, histological, neurological, behavioral, and social. The underlying problem becomes less apparent with the procession of entries in the table. In fact, it is not possible to predict the specific biochemical abnormality from information at the neurological, behavioral, or social level, exactly where the most accessible information resides.
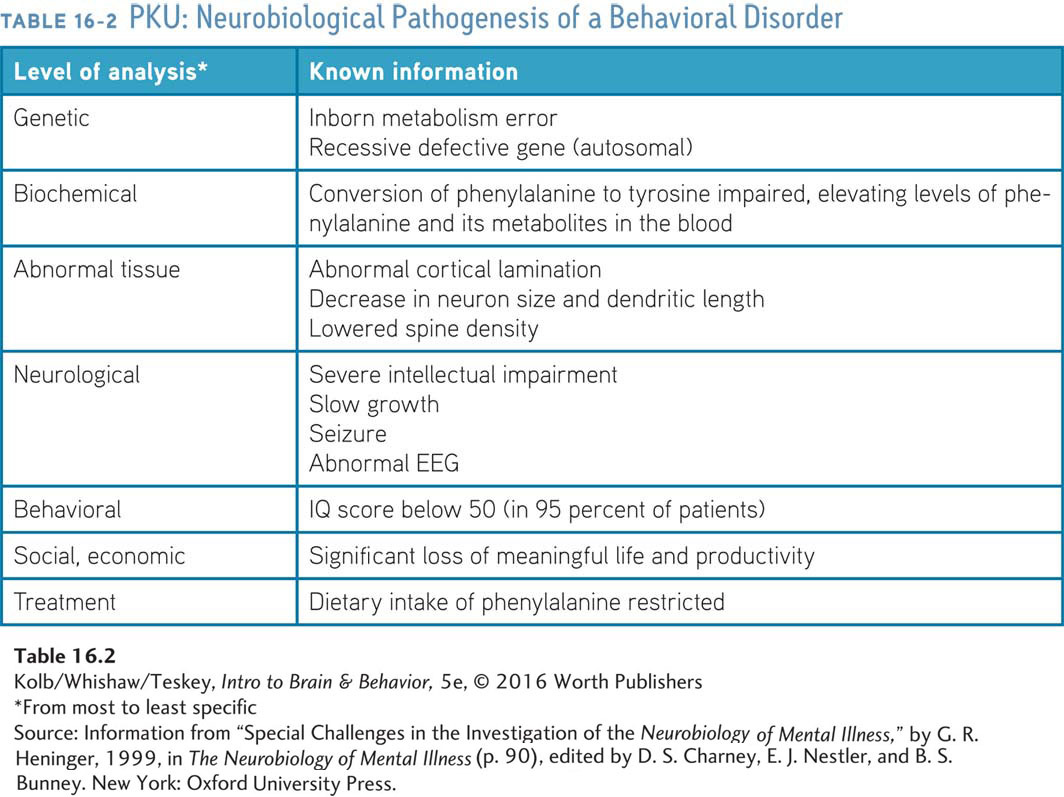
For most psychiatric diseases, the underlying pathology is unknown. For PKU, the distinctive smell of her baby’s urine detected by one mother was the first link in a chain of discoveries that identified elevated PHA. The task for future study and treatment of most behavioral disorders is to identify biological markers that will lead to similar understandings.
Challenges to Diagnosis
Knowledge about behavioral disorders is hampered by its subjective nature. Most diagnostic information gathered about a patient’s behavior comes both from patients and their families. Unfortunately, people seldom are objective observers of their own behavior or that of a loved one. We tend to be selective in noticing and reporting symptoms. If we believe someone has a memory problem, for example, we often notice memory lapses that we might ordinarily ignore.
566
Sections 14-2 and 14-3 explain a range of memory deficits.
Nor are we often specific in identifying symptoms. Simply identifying a memory problem is not sufficient. Treatment requires knowing exactly what type of memory deficit underlies the problem. Losses of memory for words, places, or habits—
Just as patients and their loved ones make diagnosis difficult, so too do diagnosticians. Behavioral information about patients may be interpreted differently by general physicians, psychiatrists, neurologists, psychologists, social workers, and others. Evaluators with different conceptual biases shape and filter the questions they ask and the information they gather.
One evaluator believes that a behavioral disorder is genetic; another believes it results from a virus; and a third, that it can be traced to repressed sexual experiences during childhood. Each makes different types of observations and administers different kinds of diagnostic tests. In contrast, diagnosing organic disorders is less dependent on subjective observations than on objective experimental methods—
Research Challenges
Even if the problems of diagnosis were solved, major obstacles to investigating behavioral disorders would still exist. Following is a partial list.
ORGANIZATIONAL COMPLEXITY The nervous system far outstrips other body systems in complexity. The brain has a wider variety of cell types than does any other body organ, and nervous system cells and their connections are plastic: they change with experience. These features add a whole new dimension to understanding healthy and disordered functioning.
Figure 5-17 summarizes major neural activating systems; Figure 6-7, how psychoactive drugs affect the GABAA receptor.
SYSTEMIC COMPLEXITY As our understanding of brain and behavior has progressed, so it has become apparent that multiple receptor systems serve widely varied functions. For example, the brain’s major activating systems, those that employ acetylcholine, dopamine, norepinephrine, serotonin, and GABA are diffuse, with little specificity between biochemistry and behavior. The neurotransmitter GABA affects some 30 percent of the brain’s synapses. When people ingest a GABA agonist, such as a benzodiazepine, multiple effects on behavior become apparent. So it is with most drug treatments, which may improve a target behavior but at the same time produce varied side effects.
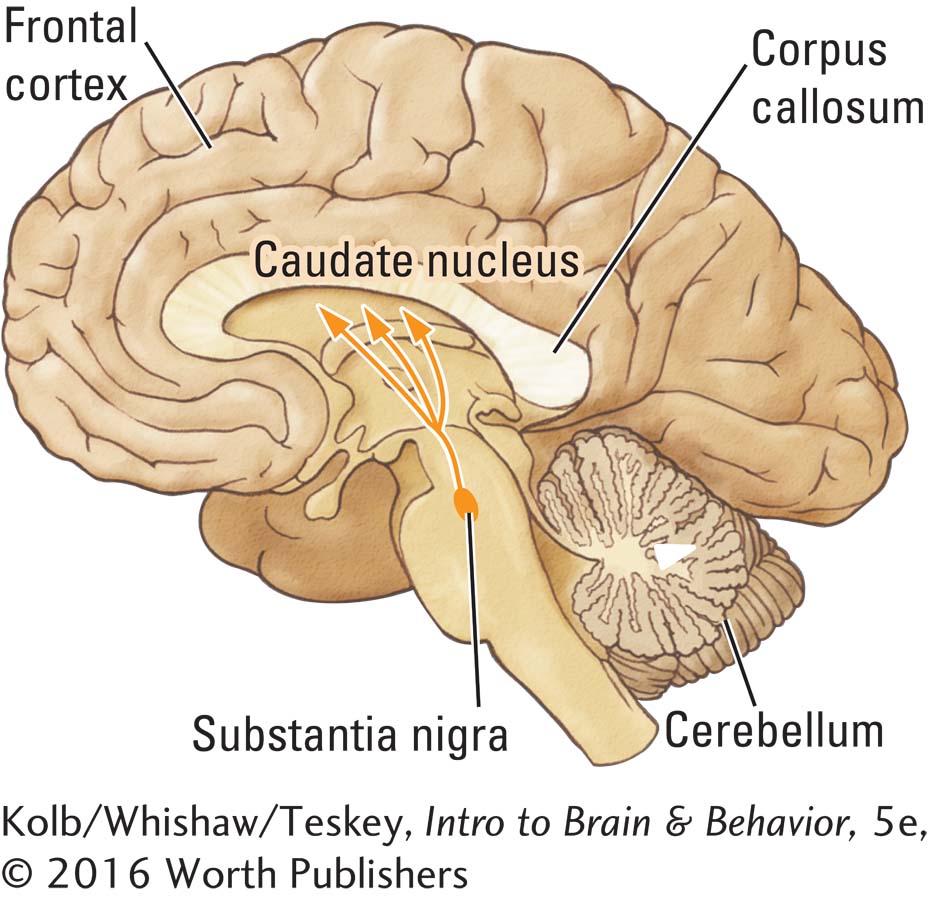
NEURONAL PLASTICITY The nervous system can adapt to extreme stress or injury. Even the nigrostriatal dopaminergic system’s close relation to Parkinson disease is enigmatic. It is impossible to tie dopamine depletion to a consistent behavioral syndrome. Two people with Parkinson disease can exhibit vastly different symptoms, even though the common basis of the disease is a loss of neurons from the substantia nigra (Fereshtehnejad et al., 2015). Further, only when the loss of dopamine neurons exceeds about 60 percent to 80 percent do investigators see clinical signs of Parkinson disease. Are those cells not all needed? That is unlikely, but the result shows that the brain’s compensatory plasticity is considerable. When a disease progresses slowly, the brain has a remarkable capacity for adapting.
567
COMPENSATORY PLASTICITY Even the best technology produces uncertain relationships. Magnetic resonance imaging may show that a person with multiple sclerosis has many nervous system lesions yet displays few outward symptoms. Just as brain lesions do not always produce behavioral symptoms, behavioral symptoms are not always linked to obvious neuropathology. Clearly, people display compensatory plasticity: they can change their behavior to adapt to neural change just as they can display disordered behavior without obvious brain pathology.
TECHNOLOGICAL RESOLUTION Some people have notable behavioral problems after a brain trauma, yet no obvious signs of brain damage appear on an MRI. An infant’s brain may seem healthy only to display severe cerebral palsy later. The resolution of a technology may lack sufficient detail to detect subtle neuronal change, such as a drop in dendritic spine density or injury so diffuse that it is hard to identify. Given the current diagnostic methods for both behavioral disorders and neuropathology, identifying disorders and their causes is seldom easy.
Section 7-7 reviews the benefits of creating animal models of disorders.
MODELING SIMPLICITY A major avenue for investigating the causes of disorders is to develop and study animal models. Rats with specific lesions of the nigrostriatal dopamine system are used to model Parkinson disease. Animal models lead to significant advances in understanding neural conditions and their treatment. But the view they provide of the neurobiology behind behavioral disorders can be oversimplified.
The fact that a drug reduces symptoms does not necessarily mean that it is acting on a key biochemical aspect of the pathology. Aspirin can get rid of a headache, but that does not mean that the headache is caused by the receptors on which aspirin acts. Similarly, antipsychotic drugs block dopamine D2 receptors, but that does not mean that schizophrenia is caused by abnormal D2 receptors. Schizophrenia quite possibly results from a disturbance in glutamatergic systems, and for some reason dopamine antagonists can rectify the abnormality.
MODELING LIMITATIONS Modeling human disorders is complex, and critical thinking is imperative when you encounter media reports about studies using animal models that point toward possible cures for human behavioral diseases. Caution applies especially to psychiatric disorders whose causes remain unknown. Further, many symptoms of disorders such as schizophrenia and anxiety are largely cognitive. Objectively identifying any cognitive processes mimicked by a laboratory model is a difficult task.
16-1 REVIEW
Multidisciplinary Research on Brain and Behavioral Disorders
Before you continue, check your understanding.
Question 1
Neural correlates of Freud’s id, ego, and superego could be, respectively, the ____________, ____________, and ____________.
Question 2
Causes of disordered behavior include ____________, ____________, ____________, ____________, and ____________.
Question 3
For most psychiatric disorders, the causes are unknown, but ____________ is an exception.
Question 4
A major challenge in diagnosing disorders is that diagnosis tends to be ____________.
Question 5
Describe a research conundrum for understanding brain injury.
Answers appear in the Self Test section of the book.