9-5 The Visual Brain in Action
314
Anatomical and physiological studies of brain systems leave one key question unanswered: How do all of the cells in these systems act together to produce a particular function? One way to answer this question is to evaluate what happens when parts of the visual system are dysfunctional. Then we can see how these parts contribute to the workings of the whole. We use this strategy to examine the neuropsychology of vision—
Injury to the Visual Pathway Leading to the Cortex
What happens when parts of the visual pathway leading from the eye to the cortex are injured? For instance, destruction of the retina or optic nerve of one eye produces monocular blindness, the loss of sight in that eye. Partial destruction of the retina or optic nerve produces a partial loss of sight in one eye, restricted to the visual field region that has severed connections to the brain.
Injuries to the visual pathway beyond the eye also produce blindness. For example, complete cuts of the optic tract, the LGN, or cortical region V1 result in homonymous hemianopia, blindness of one entire side of the visual field, as shown in Figure 9-40A. We encountered this syndrome in Focus 9-1, the story of D. B.’s lesion in region V1. Should a lesion in one of these areas be partial, as is often the case, the result is quadrantanopia, destruction of only a part of the visual field, illustrated in Figure 9-40B.
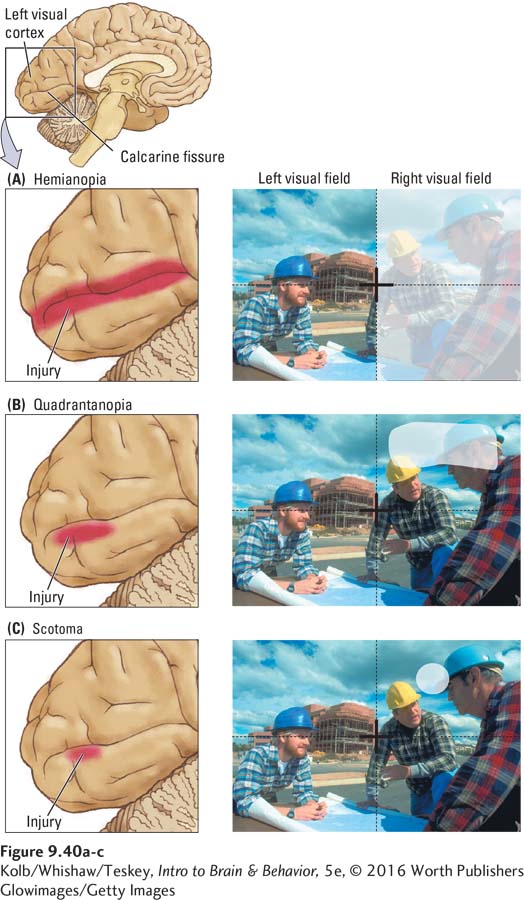
Figure 9-40C shows that small lesions in V1 often produce small blind spots, or scotomas, in the visual field. Focus 9-1 observes that scotomas can be a warning symptom for migraine sufferers. But brain-
We make tiny, involuntary eye movements almost constantly. Because of this usually constant eye motion, called nystagmus, a scotoma moves about the visual field, allowing the intact brain regions to perceive all the information in that field. If the eyes are temporarily held still, the visual system actually compensates for a scotoma through pattern completion—
The visual system may cover up a scotoma so successfully that its presence can be demonstrated to the patient only by tricking the visual system. The trick is to place an object entirely within the scotoma and without allowing the patient to shift gaze, asking what the object is. If the patient reports seeing nothing, to confirm the existence of a blind area the examiner moves the object out of the scotoma so that it suddenly appears in the intact region of the visual field.
This technique is similar to demonstrating the presence of the blind spot that is due to the optic disc (as in Figure 9-4). When a person is looking at an object with only one eye, the brain compensates for the scotoma in the same way as for the optic disc’s blind spot. As a result, the person does not notice the scotoma.
Thus the type of blindness offers clues about where in the visual pathway the cause of the problem lies. If the loss of vision is in one eye only, the problem must be in that eye or its optic nerve; if the vision loss affects both eyes, the problem most likely is in the brain. Many people have difficulty understanding why a person with damage to the visual cortex has difficulty with both eyes. They fail to realize that the visual field, not the eye, is represented in the brain.
315
Beyond region V1, the nature of visual loss caused by injury is considerably more complex. It is also very different in the ventral and dorsal streams. We therefore look at each pathway separately.
Injury to the What Pathway
We have encountered an example of damage to the what pathway: the case of D. B. in Focus 9-1. He appeared to be blind in his affected visual field but could point to the location of blinking lights in that field, suggesting that some part of his visual system was working. An even more dramatic example of ventral stream injury comes from the case of D. F., a 35-
CLINICAL FOCUS 9-4
Carbon Monoxide Poisoning
Brain damage from carbon monoxide (CO) poisoning is usually caused either by a faulty furnace or by motor vehicle exhaust fumes. The blood absorbs carbon monoxide gas, resulting in swelling and bleeding of the lungs and anoxia (loss of oxygen) in the brain. The cerebral cortex, hippocampus, cerebellum, and striatum are especially sensitive to CO-
Only a small proportion of people who are subjected to CO poisoning have permanent neurological symptoms. Among those who do, the symptoms are highly variable. Most common are cortical blindness and various agnosias, as seen in case D. F. Many also have language difficulties.
The peculiarities of the language difficulties are shown clearly in a young woman whose case was described by Norman Geschwind (1972). Geschwind studied this patient for 9 years after her accidental poisoning. She required complete nursing care during this time, never uttered spontaneous speech, and did not comprehend spoken language. Nonetheless, she could repeat with perfect accuracy sentences that had just been said to her.
She could also complete certain well-
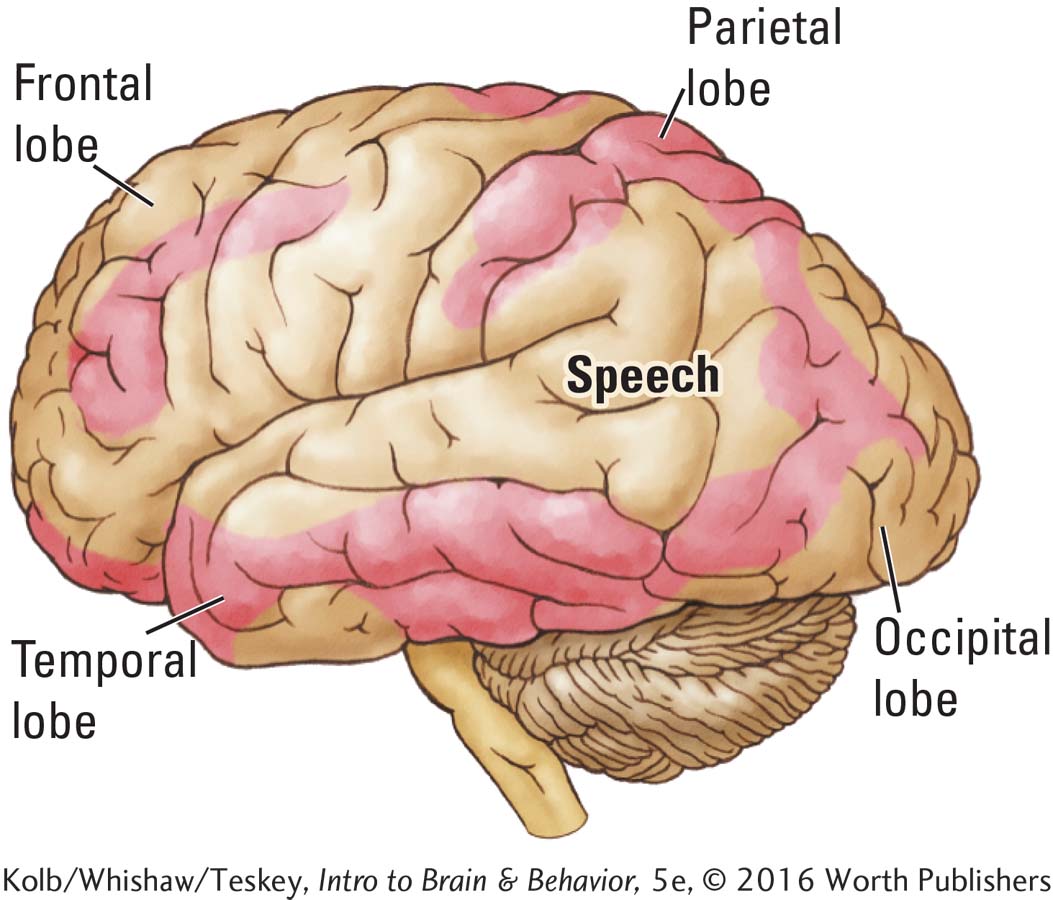
Postmortem examination of this woman’s brain found that although the parietal and temporal lobes were damaged extensively, as shown in the accompanying diagram, her speech areas were intact. Geschwind proposed that she could not comprehend speech because the words she heard did not arouse associations in other parts of her cortex.
She could, however, repeat sentences because the internal connections of the speech regions were undamaged. Geschwind did not comment on whether this woman had agnosia, but it is likely that she did. The difficulty would be in diagnosing agnosia in a person who is unable to communicate.
Areas damaged by carbon monoxide poisoning are shown in red in this postmortem diagram of Geschwind’s patient’s brain.
Section 9-2 describes damage to the temporal lobe area that causes facial agnosia.
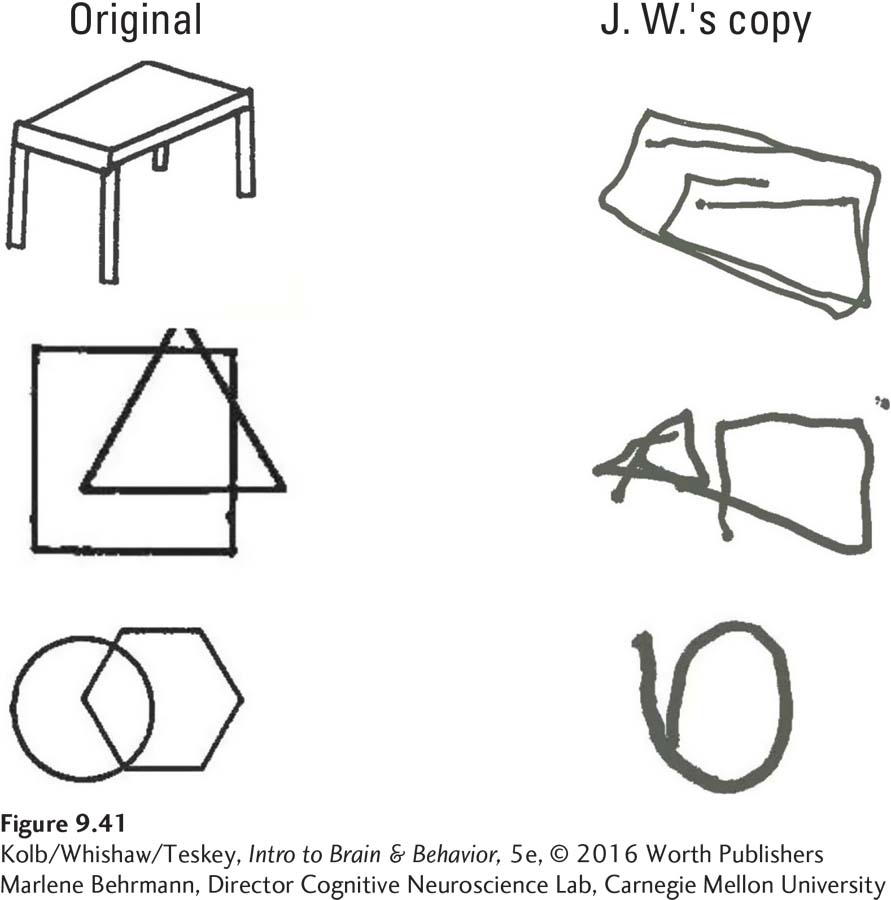
D. F.’s principal deficit was visual-
316
Clearly, D. F.’s lesion interfered with her ventral stream what pathway. Remarkably, despite her inability to identify objects or to estimate their size and orientation, D. F. retained the capacity, illustrated in Figure 9-42, to appropriately shape her hand when reaching out to grasp something. Goodale, Milner, and their research colleagues (1991) studied D. F. extensively for years and devised a way to demonstrate D. F.’s skill at reaching for objects.
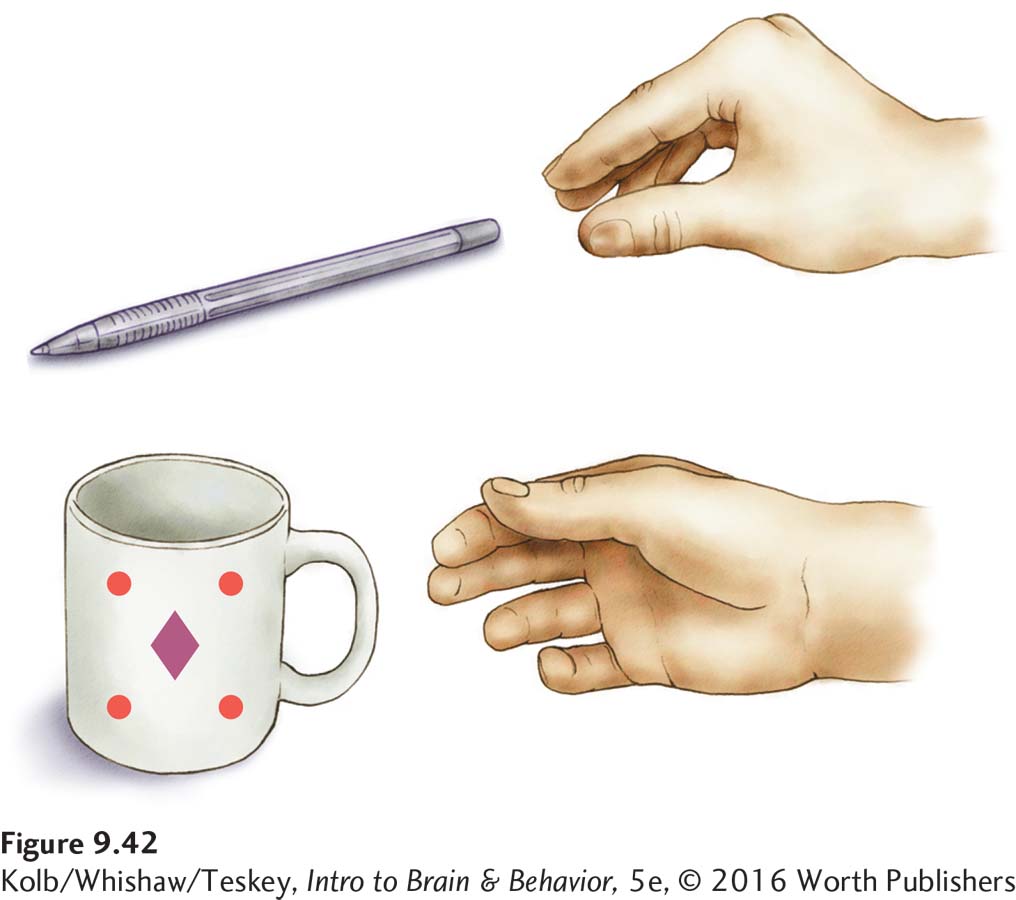
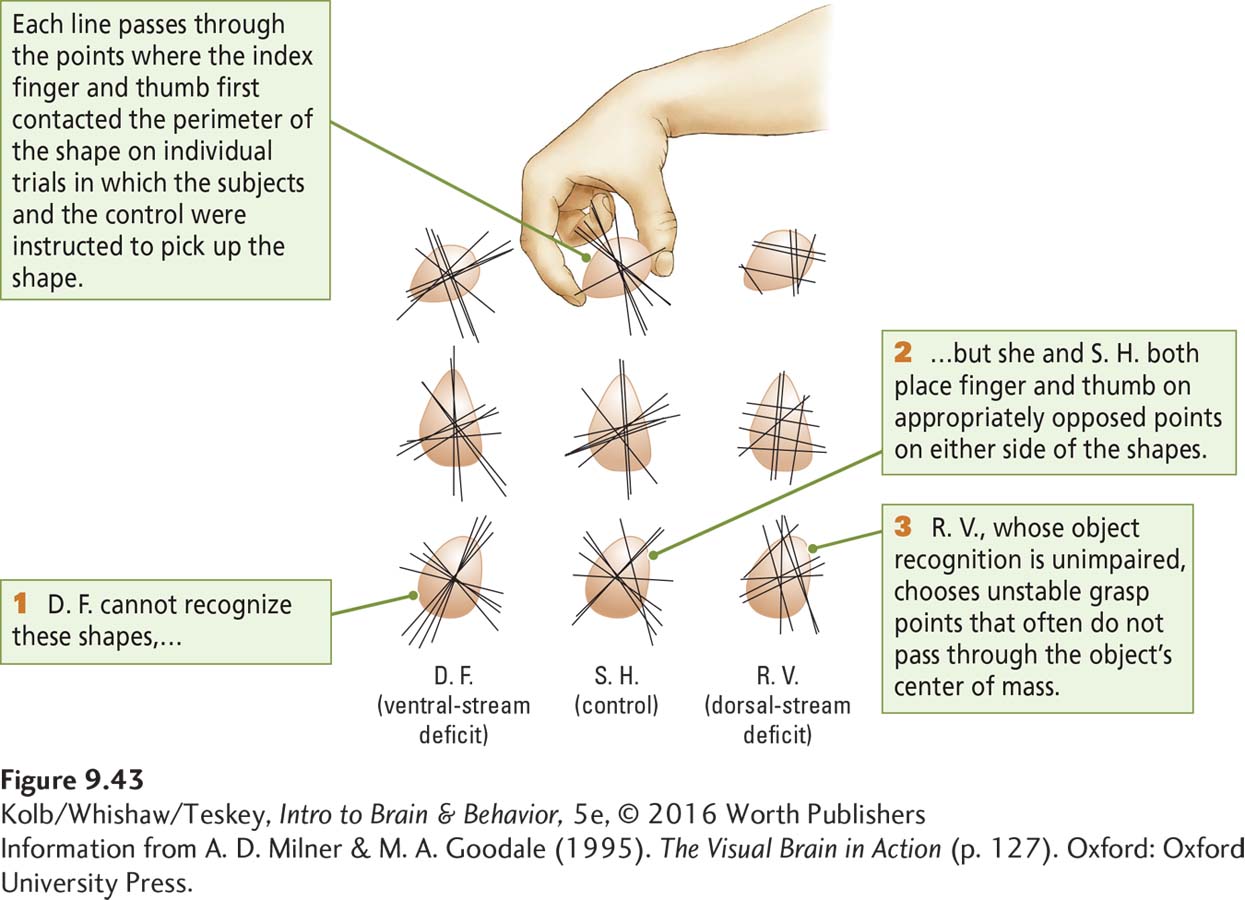
The middle column in Figure 9-43 shows the grasp patterns of a control participant (S. H.) when she picks up something irregularly shaped. S. H. grasps the object along whichever of the two axes makes it easier to pick up. When D. F. is presented with the same task, shown in the left-
Clearly, D. F. remains able to use the structural features of objects to control her visually guided grasping movements, even though she is unable to interpret these same features. This result demonstrates once more that we are consciously aware of only a small part of the sensory processing that goes on in the brain. Furthermore, D. F.’s ability to use structural features of objects for guiding movement but not for perceiving shapes again shows us that the brain has separate systems for each type of visual operation.
D. F.’s lesion is quite far back in the ventral visual pathway. More anterior lesions produce other deficits, depending on the exact location. For example, J. I., described by Oliver Sacks and Robert Wasserman (1987), was an artist who developed complete color deficiency owing to a cortical lesion presumed to be in region V4. His principal symptom was achromatopsia, or color agnosia. Despite his inability to distinguish any colors whatsoever, J. I.’s vision appeared otherwise unaffected.
Similarly, L. M., a woman described by Josef Zihl and his colleagues (1983), lost her ability to detect movement after a lesion presumed to be in region V5. In her case, objects either vanished when they moved or appeared frozen despite their movement. L. M. had particular difficulty pouring tea into a cup, because the fluid appeared to be frozen in midair. Yet she could read, write, and recognize objects, and she appeared to have normal form vision—
These varied cases demonstrate that cortical injuries in the ventral stream all somehow interfere with determining what things are or are like or are doing. In each case, the symptoms are somewhat different, however, which is thought to be indicative of damage to different subregions or substreams of the ventral visual pathway.
Injury to the How Pathway
Section 11-5 details the somatic senses, including proprioception, or body awareness.
In 1909, R. Bálint described a rather peculiar set of visual symptoms associated with a bilateral parietal lesion. The patient had full visual fields and could recognize, use, and name objects, pictures, and colors normally. But he had a severe deficit in visually guided reaching, even though he could still make accurate movements directed toward his own body (presumably guided by tactile or proprioceptive feedback from his joints). Bálint called this syndrome optic ataxia.
Since Bálint’s time, many descriptions of optic ataxia associated with parietal injury have been recorded. Goodale has studied several such patients, one of whom is a woman identified as R. V. (Milner & Goodale, 2006). In contrast with patient D. F.’s visual form agnosia, R. V.’s perception of drawings and objects was normal, but she could not guide her hand to reach for objects.
317
The rightmost column in Figure 9-43 shows that, when asked to pick up the same irregularly shaped objects that D. F. could grasp normally, R. V. often failed to place her fingers on the appropriate grasp points, even though she could distinguish the objects easily. In other words, although R. V.’s perception of an object’s features was normal for the task of describing that object, her perception was not normal for the task of visually guiding her hand to reach for the object.
To summarize, people with damage to the parietal cortex in the dorsal visual stream can see perfectly well, yet they cannot accurately guide their movements on the basis of visual information. Guidance of movement is the dorsal stream’s function. In contrast, people with damage to the ventral stream cannot perceive objects, because object perception is a ventral stream function. Yet these same people can guide their movements to objects on the basis of visual information.
The first kind of patient, like R. V., has an intact ventral stream that analyzes the visual characteristics of objects. The second kind of patient, like D. F., has an intact dorsal stream that visually directs movements. Comparing the two types of cases enables us to infer the visual functions of the dorsal and ventral streams.
9-5 REVIEW
The Visual Brain in Action
Before you continue, check your understanding.
Question 1
Cuts completely through the optic tract, LGN, or V1 produce ____________.
Question 2
Small lesions of V1 produce small blind spots called ____________.
Question 3
Destruction of the retina or the optic nerve of one eye produces ____________.
Question 4
The effect of severe deficits in visually guided reaching is called ____________.
Question 5
Contrast the effects of injury to the dorsal stream and the effects of injury to the ventral stream.
Answers appear in the Self Test section of the book.