In codominance, both alleles at a locus are expressed
Sometimes the two alleles at a locus produce two different phenotypes that both appear in heterozygotes, a phenomenon called codominance. Note that this is different from incomplete dominance, where the phenotype of a heterozygote is an intermediate between the phenotypes of the parents. A good example of codominance is seen in the ABO blood group system in humans (this is also an example of multiple alleles).
252
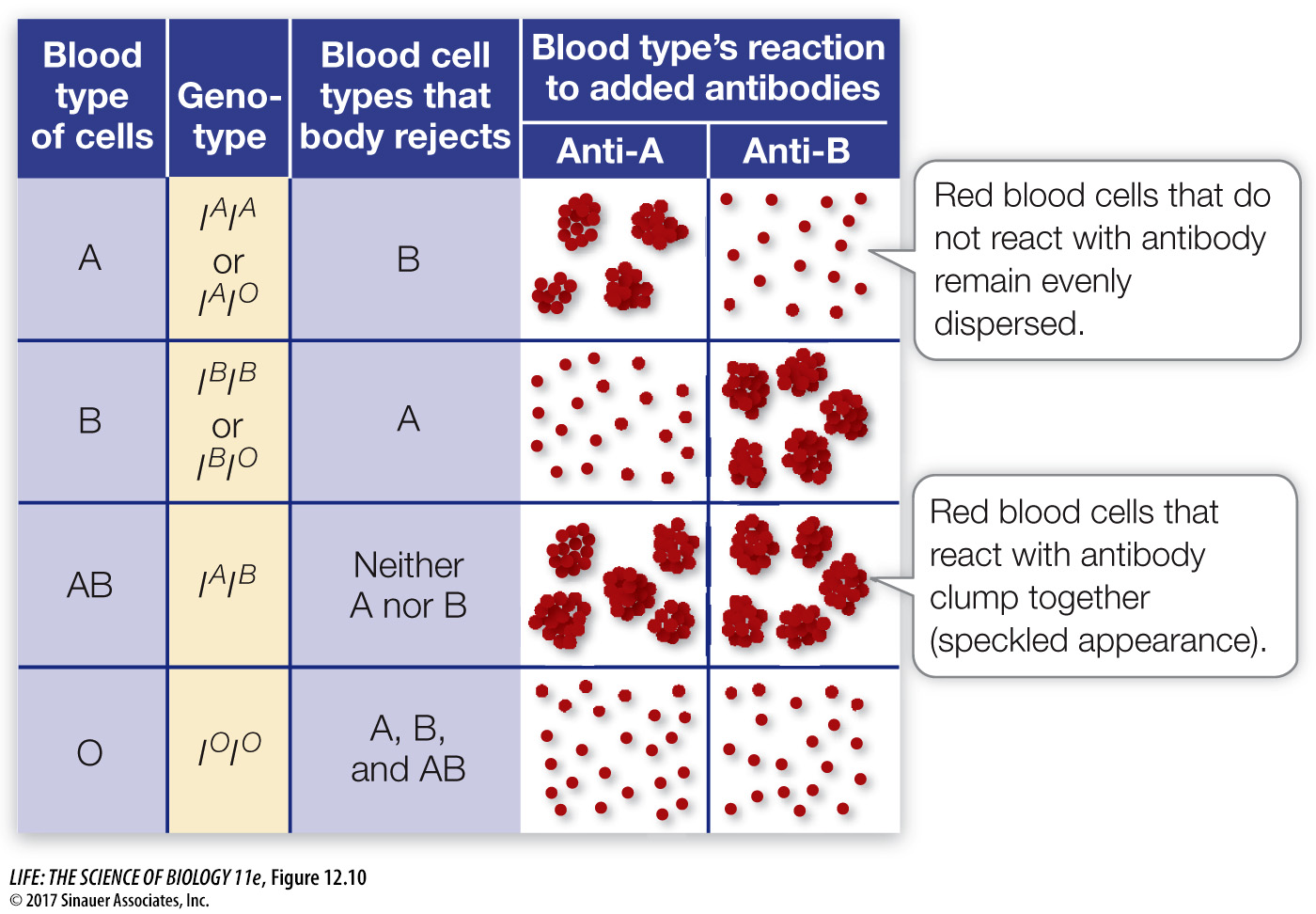
Early attempts at blood transfusion frequently killed the patient. Around 1900, the Austrian scientist Karl Landsteiner mixed blood cells and serum (blood from which cells have been removed) from different individuals. He found that only certain combinations of blood and serum are compatible. In other combinations, the red blood cells from one individual form clumps in the presence of serum from the other individual, a discovery that led to our ability to administer compatible blood transfusions that do not kill the recipient.
Clumps in mixed blood form as a consequence of mechanisms of the immune system that protect the body from invasion by “nonself” molecules or organisms. Specific proteins in human serum, called antibodies, react with foreign molecules or particles. The specific part of a molecule that is recognized by an antibody is called an antigen. Oligosaccharides on the surfaces of red blood cells can function as antigens. For example, people with type A blood make the A antigen, and those in the B group make the B antigen; A and B antigens are specific oligosaccharides on the surfaces of their red blood cells. If a person with type A blood is given a transfusion of type B blood, that individual’s immune system will recognize the B antigen as nonself and make antibodies against it (Figure 12.10). Likewise, a person with type B blood will make antibodies against the A antigen. However, someone with the codominant AB blood type makes both the A and the B antigens and will not make antibodies against either antigen. So a person with type AB blood can receive a transfusion from just about anyone. Individuals with type O blood make neither the A nor the B antigen (see Figure 12.10); they can receive blood only from a type O individual but can donate blood to individuals of any ABO blood group.
The oligosaccharides on the surfaces of red blood cells are made by enzymes that catalyze the formation of bonds between specific sugars. The ABO genetic locus encodes one such enzyme and has three alleles, IA, IB, and IO, each producing a different version of the enzyme. The product of the IA allele adds N-acetylgalactosamine to the end of a pre-
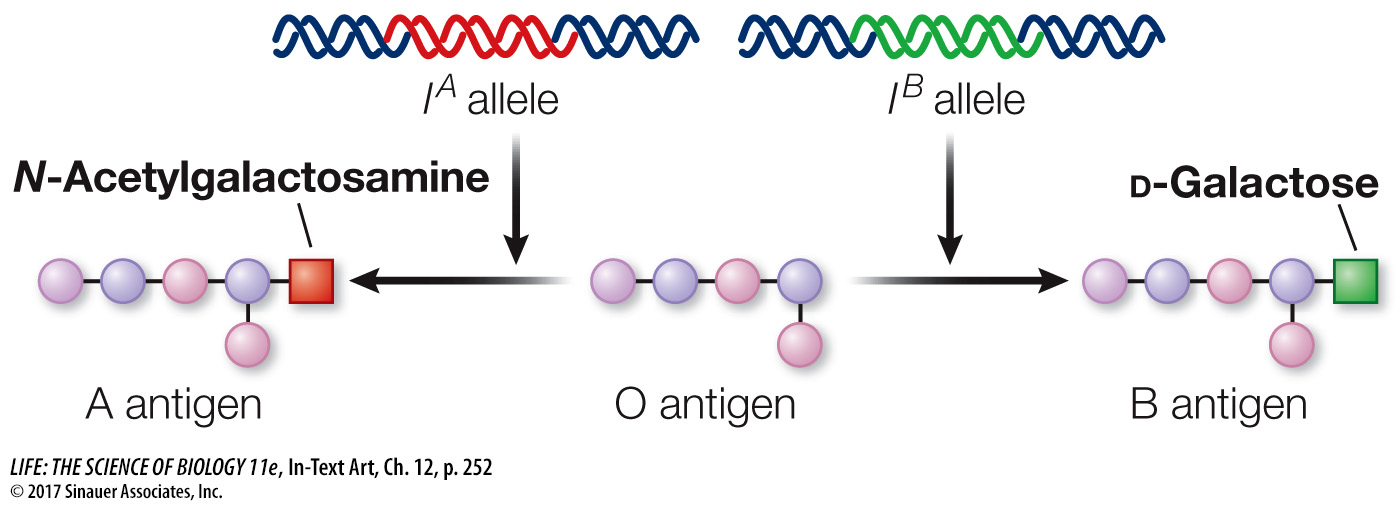
Since people inherit one allele from each parent, they may have at the ABO locus any combination of these alleles: IAIB, IAIO, IAIA, and so on. The IA and IB alleles are codominant because a person with both alleles makes both the A and the B antigens, and both kinds of oligosaccharide occur on their red blood cells. You’ll learn more about the functions of antibodies and antigens in Chapter 42.