Vaccines are an application of immunological memory
Thanks to immunological memory, exposure to many diseases (including childhood diseases such as chicken pox) provides a natural immunity to those diseases. Furthermore, it is possible to provide artificial immunity against many life-
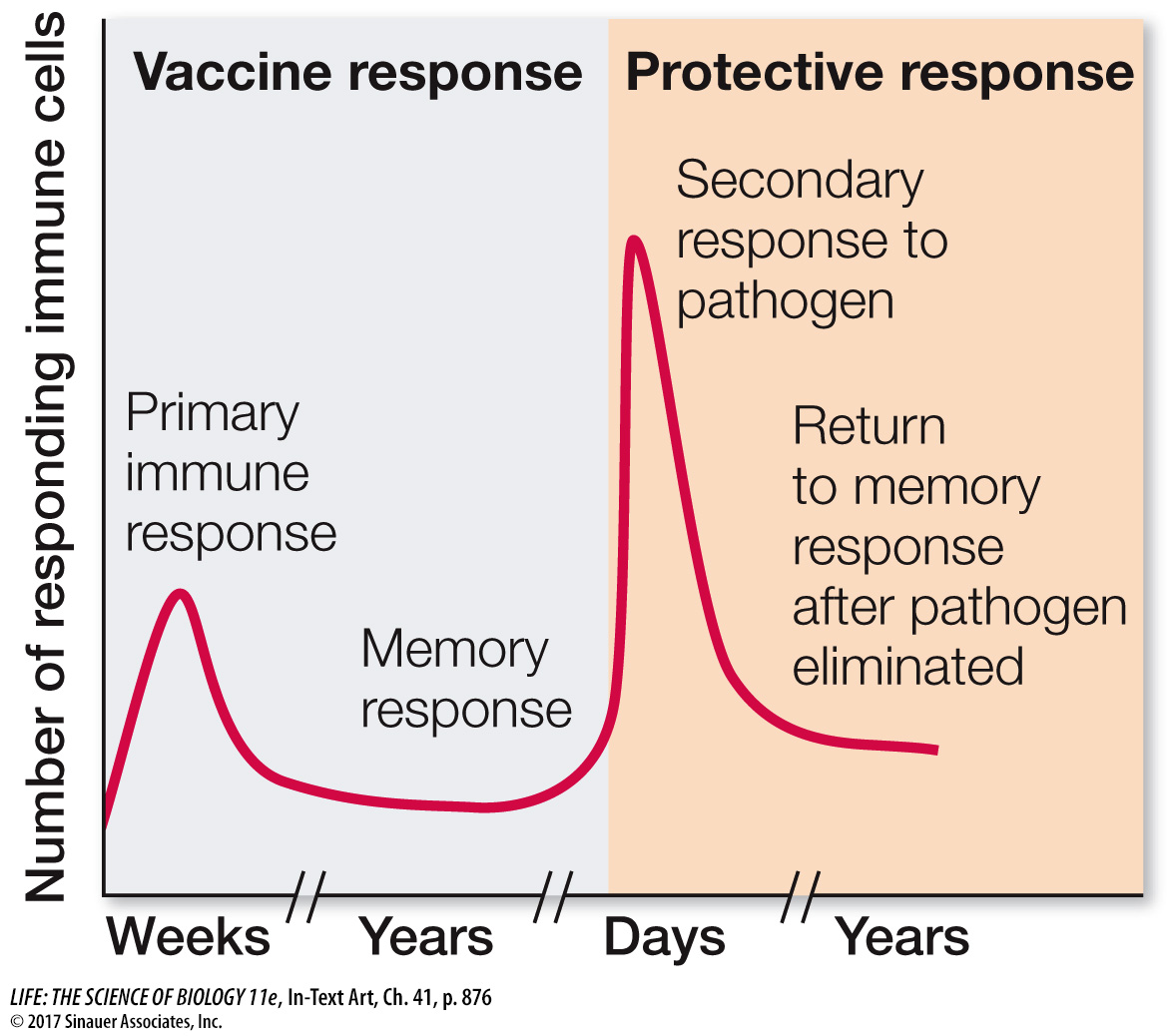
Vaccination initiates a primary immune response, generating memory cells without making the person ill. Later, if a pathogen carrying the same antigen attacks, specific memory cells already exist. They recognize the antigen and quickly overwhelm the invaders with a massive production of lymphocytes and antibodies.
Because of mutation, an antigenic determinant on a pathogen can change over time. If the change is significant in terms of three-
877
investigating life
What Are the Mechanisms and Implications of Long-
experiment
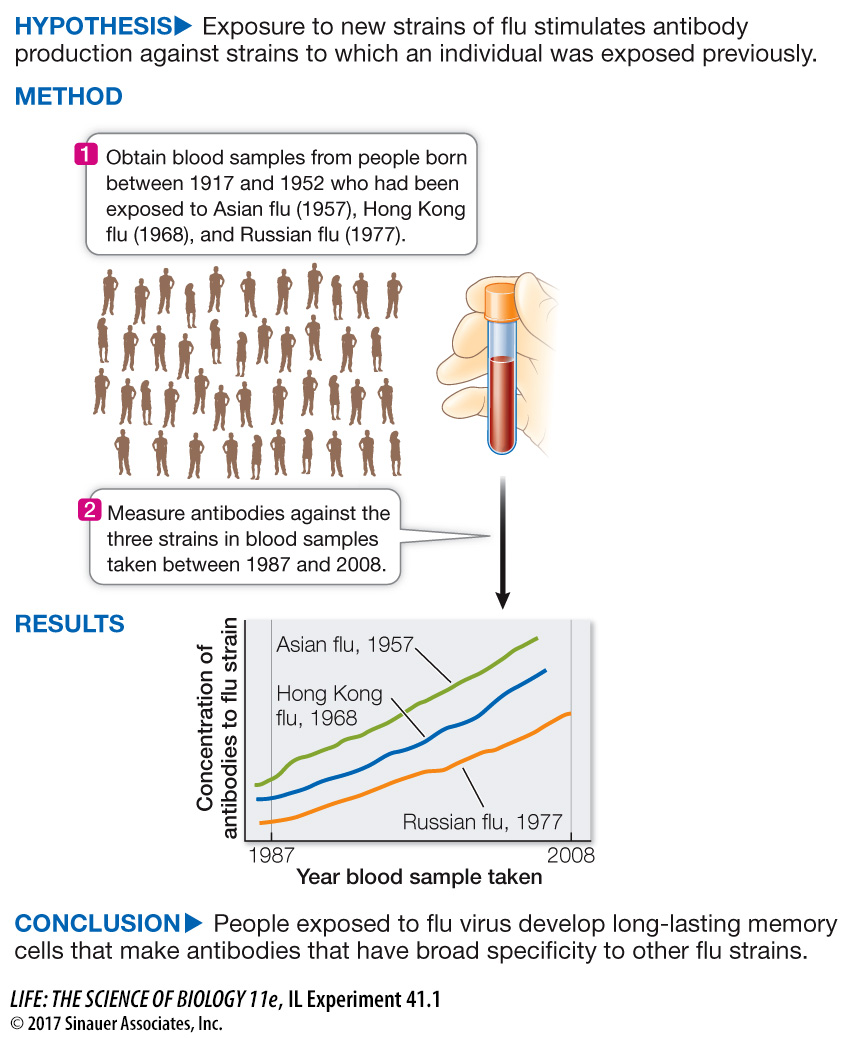
Original Paper: Miller, M. et al. 2013. Neutralizing antibodies against previously encountered influenza virus strains increase over time: A longitudinal analysis. Science Translational Medicine 5: 1–
The Framingham Heart Study was begun in 1948 with the objective of finding out the causes of heart disease and stroke. About 5,000 people ages 30–
878
work with the data
QUESTIONS
Question 1
Blood samples were taken from 1987 to 2008, and the people’s reactivity against various flu strains was tested. The results for antibodies against the Russian flu strain of 1977 in numerous individuals are shown in Figure A. Note that these people were exposed to many flu strains after 1977. The data shown are typical for the way specific immune reactions are measured. The titer is presented as a reciprocal. For example, a titer of 2 means that undiluted serum sample gave an antibody reaction (titer 1), and so did a dilution of 1 part serum and 1 part water (dilution of 1/2, reciprocal = 2). If the sample was diluted to a titer of 4 (1 part serum, 3 parts water), there was no reaction because the concentration of antibody was too low. The higher the titer number, the more the blood serum could be diluted to still react with the antigen; that is, a higher titer number means that there were more antibodies in the original serum sample. What can you conclude about the titer of anti-
While some people had low titers and other had high titers of anti-
Question 2
The flu virus mutates rapidly. In contrast, another virus to which people are exposed, cytomegalovirus (CMV), does not mutate rapidly. Antibody titer against CMV were measured, and the data are shown in Figure B. What can you conclude from these data? Compare the antibody response to CMV over time with that against the Russian flu virus strain and comment.
There was little change in the antibody titers to CMV. Note that the y axis is much lower quantitatively in this case than the y axis for anti-
Question 3
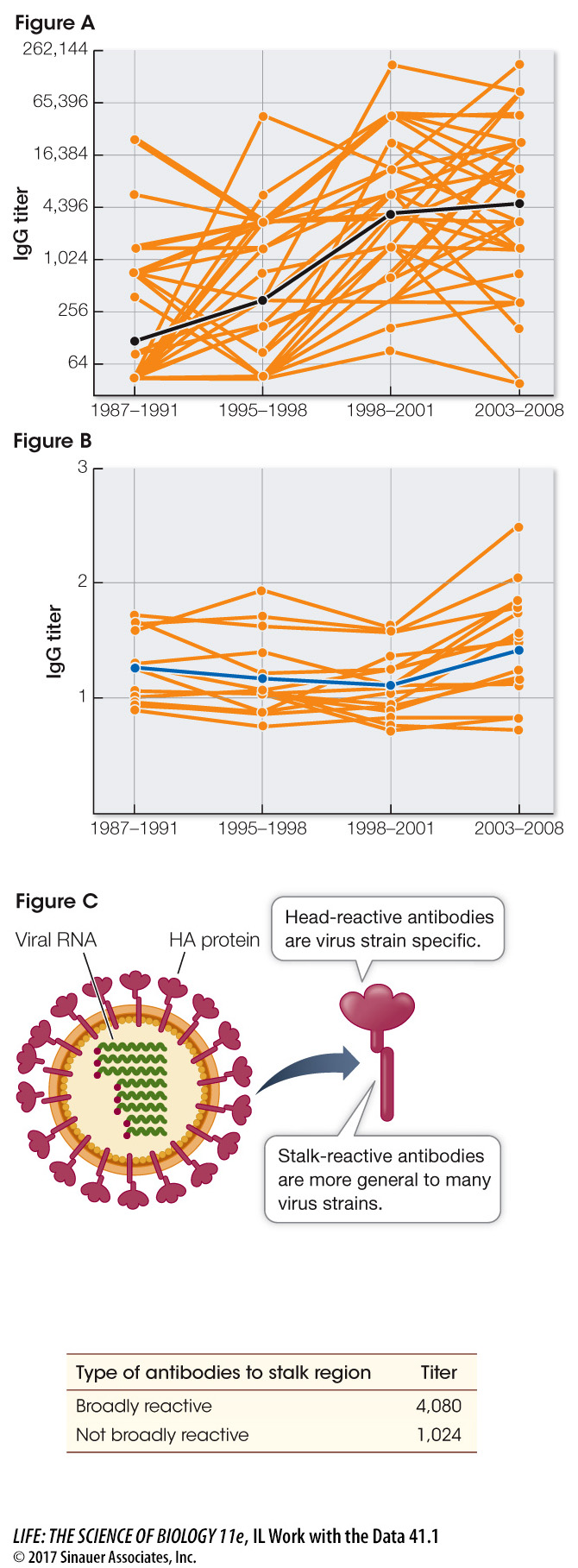
A protein on the surface of the flu virus called hemagluttinin (HA) is exposed to the immune system because of its prominent location (Figure C). When the flu virus genes mutate, the “head” of the protein tends to accumulate more changes than the stalk. Thus the amino acid sequences of stalk regions of various flu strains are similar. The investigators measured antibodies to the stalk region that were either broadly reactive to various flu strains, or not broadly reactive. The results are shown in the table. What can you conclude about the broadly reactive antibodies? How does this provide a guide for the development of a broadly based flu vaccine?
The antibodies that developed were mostly broadly reactive. These antibodies could be used to develop a vaccine that might work on old as well as new strains of flu virus.
A similar work with the data exercise may be assigned in LaunchPad.
As you saw in the opening story, vaccination has completely or almost completely wiped out some deadly diseases in industrialized countries.