Smooth muscle causes slow contractions of many internal organs
Smooth muscle provides the contractile force for most of our internal organs, which are under the control of the autonomic nervous system. Smooth muscle moves food through the digestive tract, controls the flow of blood through blood vessels, and empties the urinary bladder. Smooth muscle also generates “goose bumps” on the skin and causes the hair on the back of a dog or cat to stand erect when the animal is being aggressive or defensive. Structurally, smooth muscle cells are the simplest muscle cells. They are smaller than skeletal muscle cells, usually long and spindle-shaped, and each has a single nucleus. They are “smooth” because the actin and myosin filaments are not as regularly arranged as they are in skeletal and cardiac muscle, and so do not produce the striated appearance.
Some smooth muscle tissue, such as that from the wall of the digestive tract, is arranged in sheets, and individual cells in a sheet are in electrical contact with one another through gap junctions, as they are in cardiac muscle. As a result, an action potential generated in one smooth muscle cell spreads to all the cells in that sheet of tissue, and the sheet contracts in a coordinated fashion.
The cell membranes of smooth muscle cells are sensitive to stretch, with important consequences. For example, if the wall of the digestive tract is stretched in one location (as by a mouthful of food passing down the esophagus to the stomach), the membranes of the stretched cells depolarize, reach threshold, and fire action potentials, which cause the cells to contract. Thus smooth muscle contracts after being stretched, and the harder it is stretched, the stronger it contracts. This behavior of smooth muscle is important for moving food through the digestive system.
The walls of blood vessels—except capillaries—are smooth muscle. This is especially true on the arterial side where the blood is under higher pressure. Changes in vascular smooth muscle tone are responsible for controlling the distribution of blood in the body.
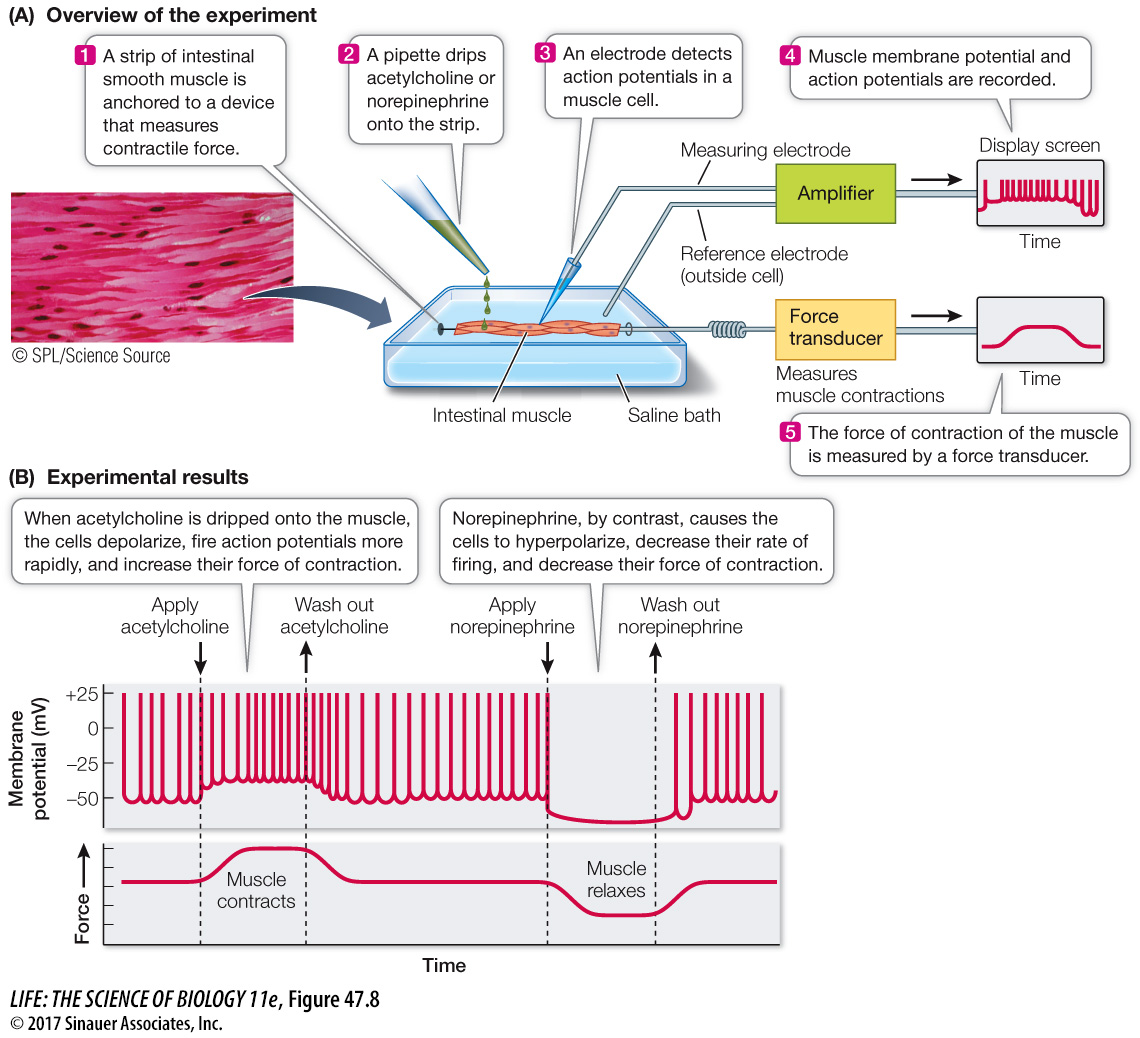
The neural influences on smooth muscle come from the two divisions of the autonomic nervous system (see Figure 46.8). The neurotransmitters of the sympathetic and parasympathetic postganglionic cells alter the membrane potential of smooth muscle cells. For example, in the digestive tract, acetylcholine causes smooth muscle cells to depolarize, making them more likely to fire action potentials and contract. Antagonistically, norepinephrine causes these muscle cells to hyperpolarize and thus be less likely to fire action potentials and contract (Figure 47.8B). In contrast, norepinephrine acting through G protein-linked receptors causes the smooth muscle in arteries serving the gut to contract. Remember that the action of the neurotransmitters depends on the receptors in the target tissues. Sympathetic activity is high in a fight-or-flight situation; in an emergency you don’t need to digest your lunch, but it could help to shunt blood to the tissues critical for survival.
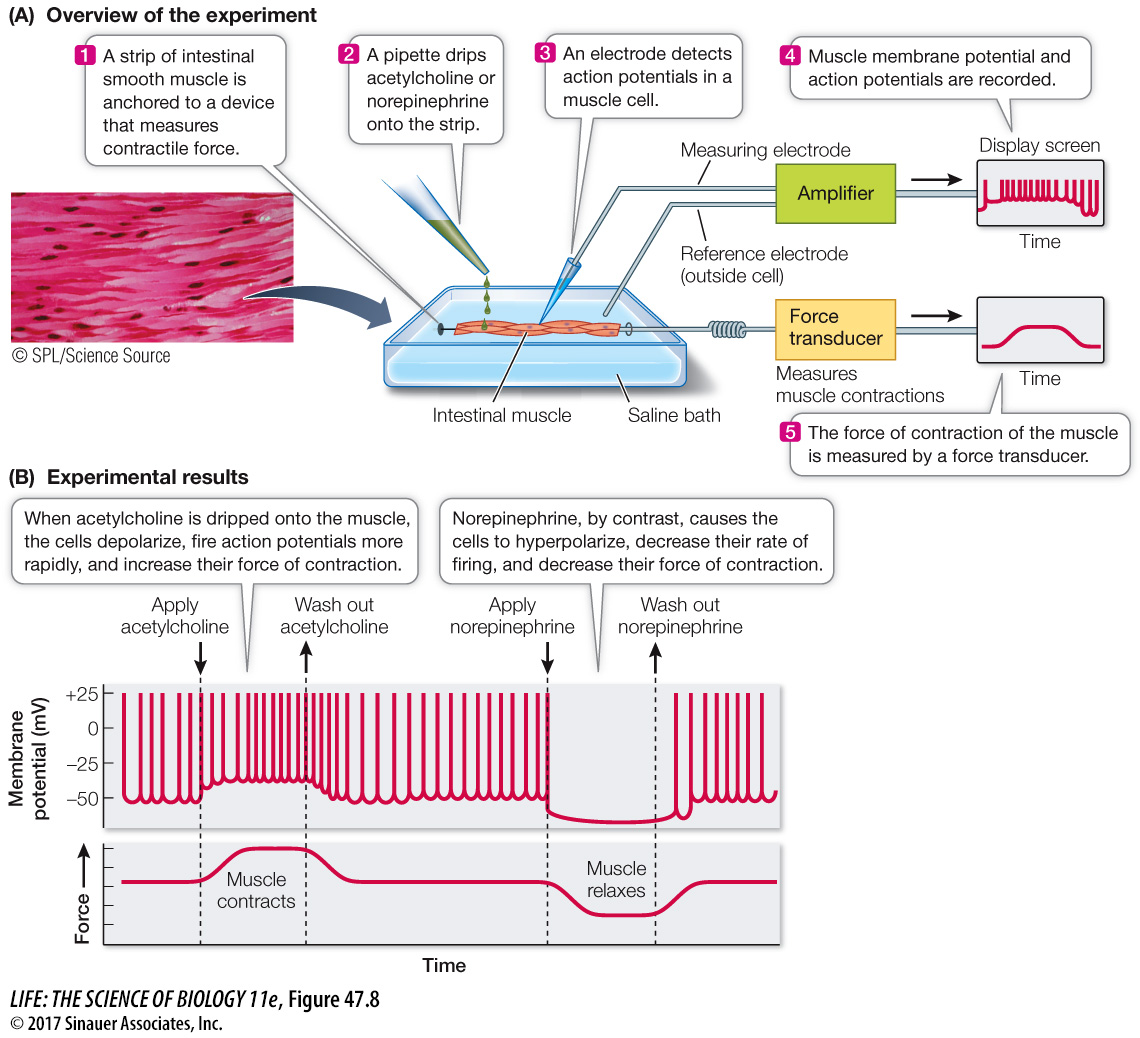
Figure 47.8 How do Autonomic Nervous System Neuro-transmitters Control the Firing Rate of Smooth Muscle Cells? (A) When a strip of intestinal smooth muscle is mounted in an incubation bath so that its generation of action potentials and its force of contraction can be recorded, it is possible to test the effects of sympathetic and parasympathetic neurotransmitters on that tissue. (B) Acetylcholine depolarizes (makes less negative) the membranes and increases action potentials; norepinephrine hyperpolarizes (makes more negative) the membranes and decreases action potentials.
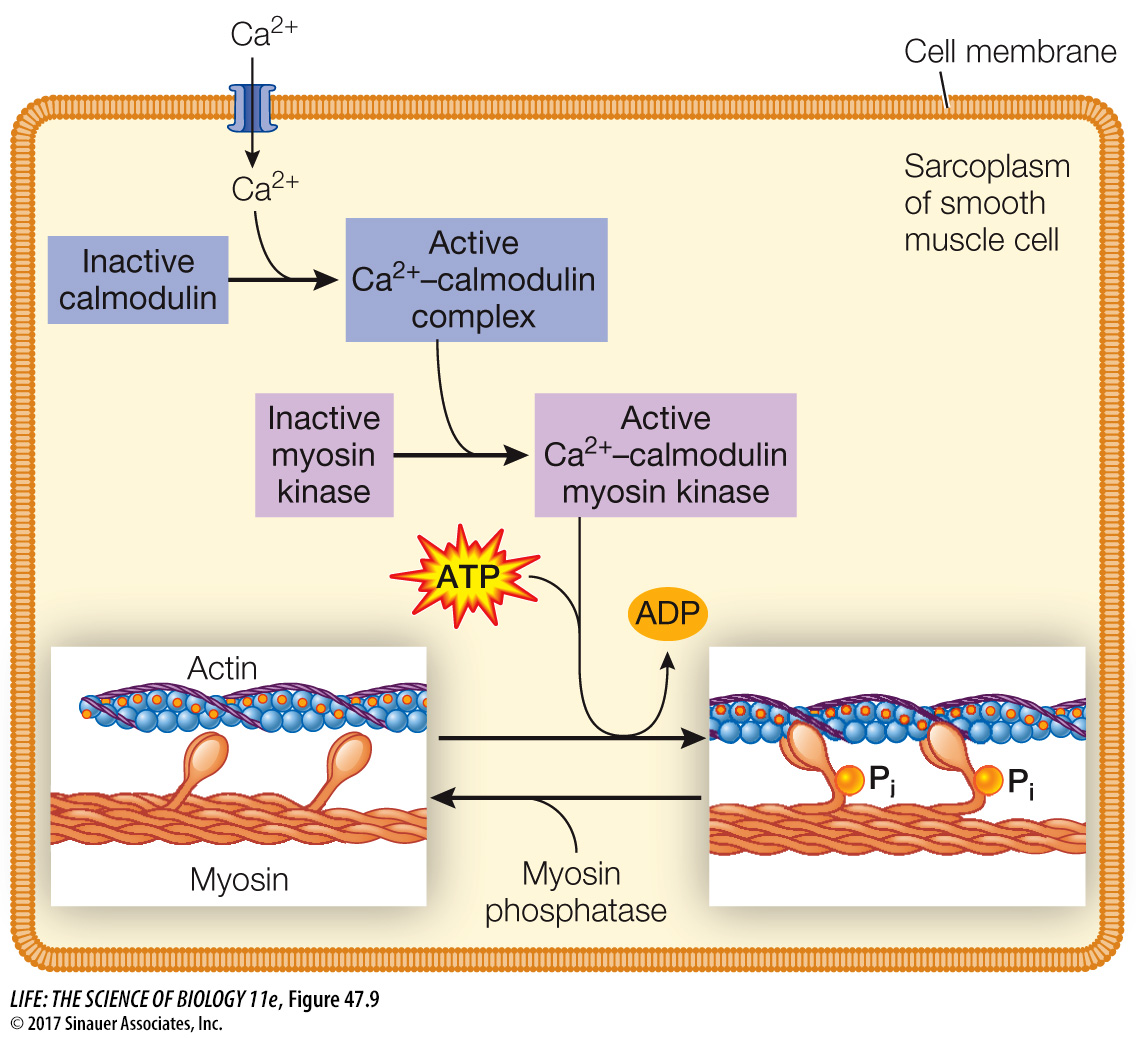
Smooth muscle cell contraction is not controlled by the troponin–tropomyosin mechanism, but calcium still plays a critical role. A Ca2+ influx into the sarcoplasm of a smooth muscle cell can be stimulated by action potentials, hormones, or stretching. The Ca2+ that enters the sarcoplasm combines with a protein called calmodulin. The Ca2+–calmodulin complex activates an enzyme called myosin kinase that phosphorylates myosin heads. When the myosin heads in smooth muscle are phosphorylated, they undergo cycles of binding and releasing actin, causing muscle contraction. As Ca2+ is removed from the sarcoplasm, it dissociates from calmodulin, and the activity of myosin kinase falls. An additional enzyme, myosin phosphatase, dephosphorylates the myosin to help reduce actin–myosin interactions (Figure 47.9).
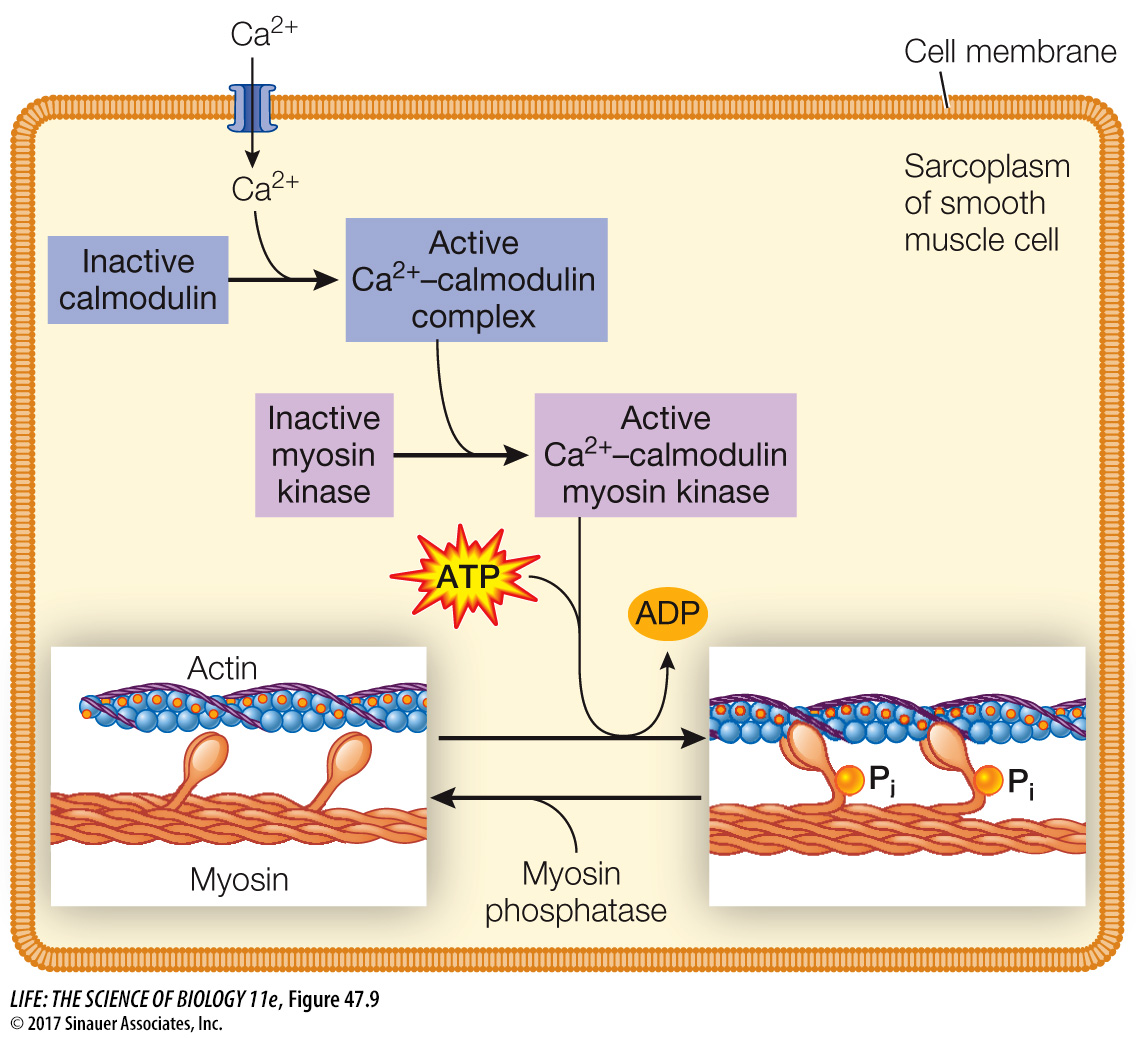
Figure 47.9 The Role of Ca2+ in Smooth Muscle Contraction When a smooth muscle cell is depolarized by a neurotransmitter, Ca2+ enters the sarcoplasm and binds to calmodulin, which in turn activates an enzyme that phosphorylates the myosin heads, causing them to bind to actin. As long as the myosin remains phosphorylated, actin and myosin go through cycles of binding and release. Thus in smooth muscle the Ca2+-mediated change is on myosin, whereas in skeletal and cardiac muscle it is on the actin–tropomyosin filament.
Animation 47.2 Smooth Muscle Action