Tidal ventilation produces dead space that limits gas exchange efficiency
Lungs evolved in early lungfishes as outpocketings of the digestive tract. Although lung structure has evolved considerably, lungs remain dead-
A flowmeter measures the volume of air breathed in and out (Figure 48.9). Using a human as an example, the amount of air that moves either in or out per breath when at rest is called the tidal volume (TV) (about 500 mL for an average human adult). When we breathe in as much as possible, the additional volume is the inspiratory reserve volume (IRV). Conversely, if we forcefully exhale as much air as possible, the additional amount of air expelled is the expiratory reserve volume (ERV). The maximum capacity for air exchange in one breath, or the vital capacity (VC), is the sum of TV + IRV + ERV. The vital capacity of an athlete is generally greater than that of a nonathlete, and vital capacity decreases with age because of stiffening of the lung tissue.
research tools
Figure 48.9A Measuring Lung Ventilation A flowmeter is a device that measures the volume of air a person breathes through a mouthpiece. The combined tidal volume, inspiratory reserve volume, and expiratory reserve volume are the lungs’ vital capacity. The vital capacity plus the residual volume are the total lung capacity.
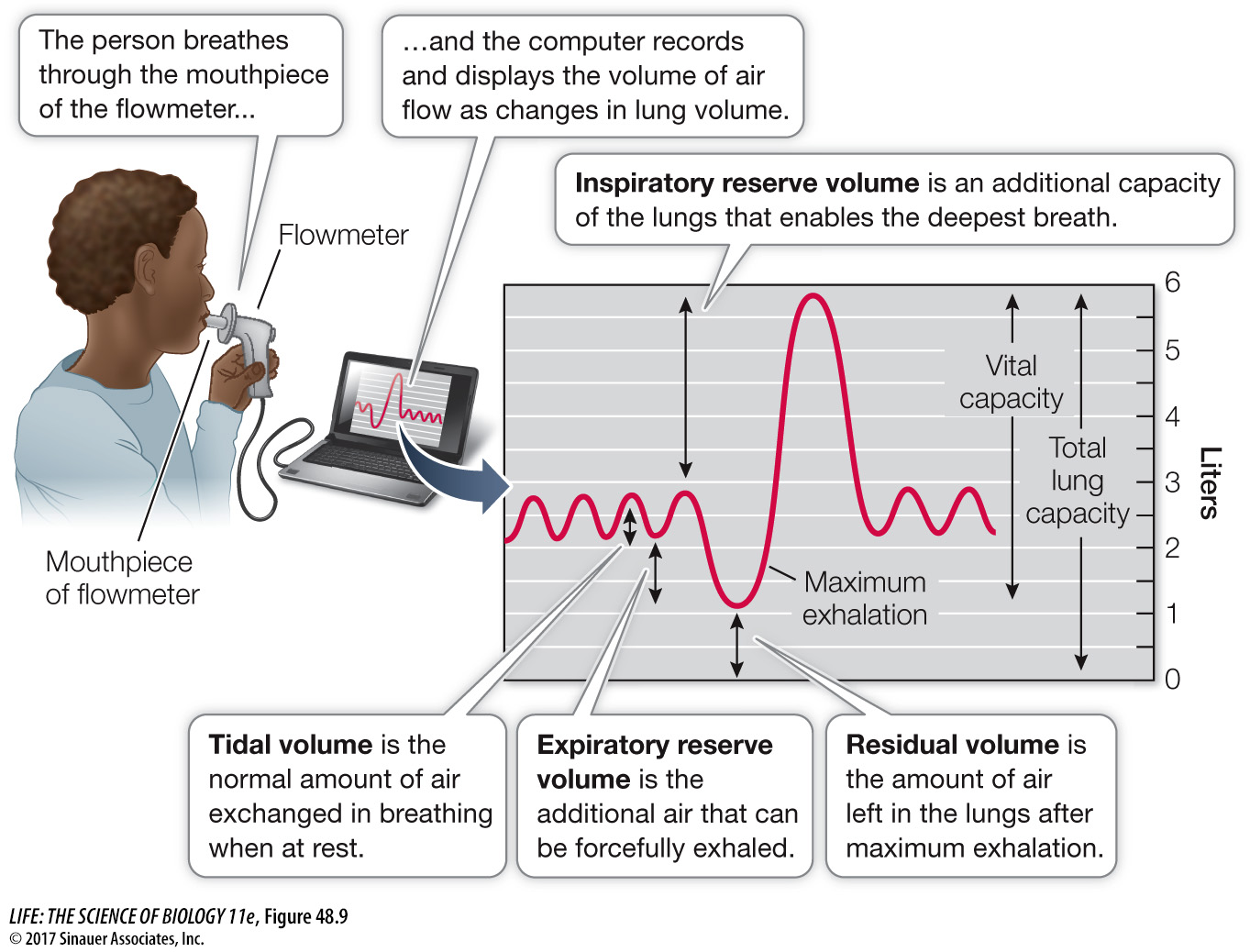
Vital capacity is not the entire lung capacity because of the dead space, also called the residual volume (RV). We can’t measure RV directly with the flowmeter, but we can measure it indirectly using the helium dilution method. The flowmeter is attached to a closed reservoir of air of a known volume (Vres) so that a person can breathe in and out from that reservoir. If this reservoir has a known amount of helium (He) in it, and a subject breathes the air in that reservoir through several breathing cycles, the helium will become distributed in the reservoir and in the subject’s respiratory system. Helium is not absorbed into the body from the lungs, so the total amount of helium at the beginning of a test (Hei) will equal the total amount at the end of the test (Hef)—it will just be distributed over a larger volume and therefore be less concentrated. The following formula quantifies that relationship:
Initial amount of He = final amount of He
1030
work with the data
Figure 48.9B Measuring Lung Ventilation
A patient complains of always being short of breath. Using a flowmeter, the physician determines that the patient’s tidal volume is 0.3 L and his expiratory reserve volume is 1.5 L. The physician decides to use the Fick dilution method to measure the patient’s residual volume. She attaches the flowmeter to a 30-
QUESTIONS
Question 1
What is the patient’s residual volume?
Since helium is not absorbed by the respiratory system, the amount of helium remains the same after breathing from the air reservoir as before, but it is distributed in both the reservoir air and the functional residual volume (FRV) of the patient. Using the helium dilution method, we can calculate the FRV.
0.050 × 30 L = 0.044 (30 L + FRV)
1.50 L = 1.32 L + 0.044 × FRV
(1.5 - 1.32)/0.044 = FRV = 4.1 L
Subtracting the expiratory reserve volume of 1.5 L gives a residual volume of 2.6 L.
Question 2
Why do you think the patient complains of always being short of breath?
The patient is always short of breath because the the PO2 in his alveoli is seriously diminished by the stale air in his very large residual volume as well as in his increased FRV during tidal breathing.
A similar work with the data exercise may be assigned in LaunchPad.
We start the subject breathing from the reservoir at an end-
Vres × [He]i = (Vres + FRV) × [He]f
Since we can measure the ERV with the flowmeter, we can subtract the ERV from the FRV to obtain the RV.
Why is the RV important? Referring to Figure 48.9, you will see that for a normal person the ERV is about 1,000 mL and the RV is 1,000 mL. Thus the FRV is 2,000 mL, but the tidal volume is only 500 mL; this means that the air that reaches the alveoli (the actual gas exchange surfaces) with each breath consists of only 500 mL of fresh air diluted by 2,000 mL of stale air. The maximumPO2 in this mixed air is much below thePO2 of the outside air, and because of the tidal ventilation pattern, the PO2 in the alveoli is steadily dropping during the breathing cycle. The RV is important because it contributes to the FRV and to the dilution of the O2 in the inhaled air. Any disease or condition that increases the RV (such as emphysema or pulmonary fibrosis) compromises a patient’s respiratory ability. Similarly, considering the mixing of fresh air with the FRV, you can understand why reductions in tidal volume can be a problem—