Lungs are ventilated by pressure changes in the thoracic cavity
Human lungs are suspended in the thoracic cavity, a closed compartment bounded on the bottom by a sheet of muscle called the diaphragm (see Figure 48.10A). Each lung is covered by a continuous sheet of tissue called the pleural membrane that also lines the thoracic cavity adjacent to the lung. A thin film of fluid between the pleural membranes of the lung and the thoracic cavity lubricates the inner surfaces of the pleural membranes so they can slip and slide against each other. As with surface tension, there are forces of attraction between the molecules of fluid covering the pleural membranes. As a result, it is difficult to pull the pleural membranes apart. Think of two wet panes of glass or two wet microscope slides; you can slide them past each other, but it is difficult to separate them. While the inner surfaces of the pleural membranes are “stuck” to each other by surface tension, they can move relative to each other during breathing movements.
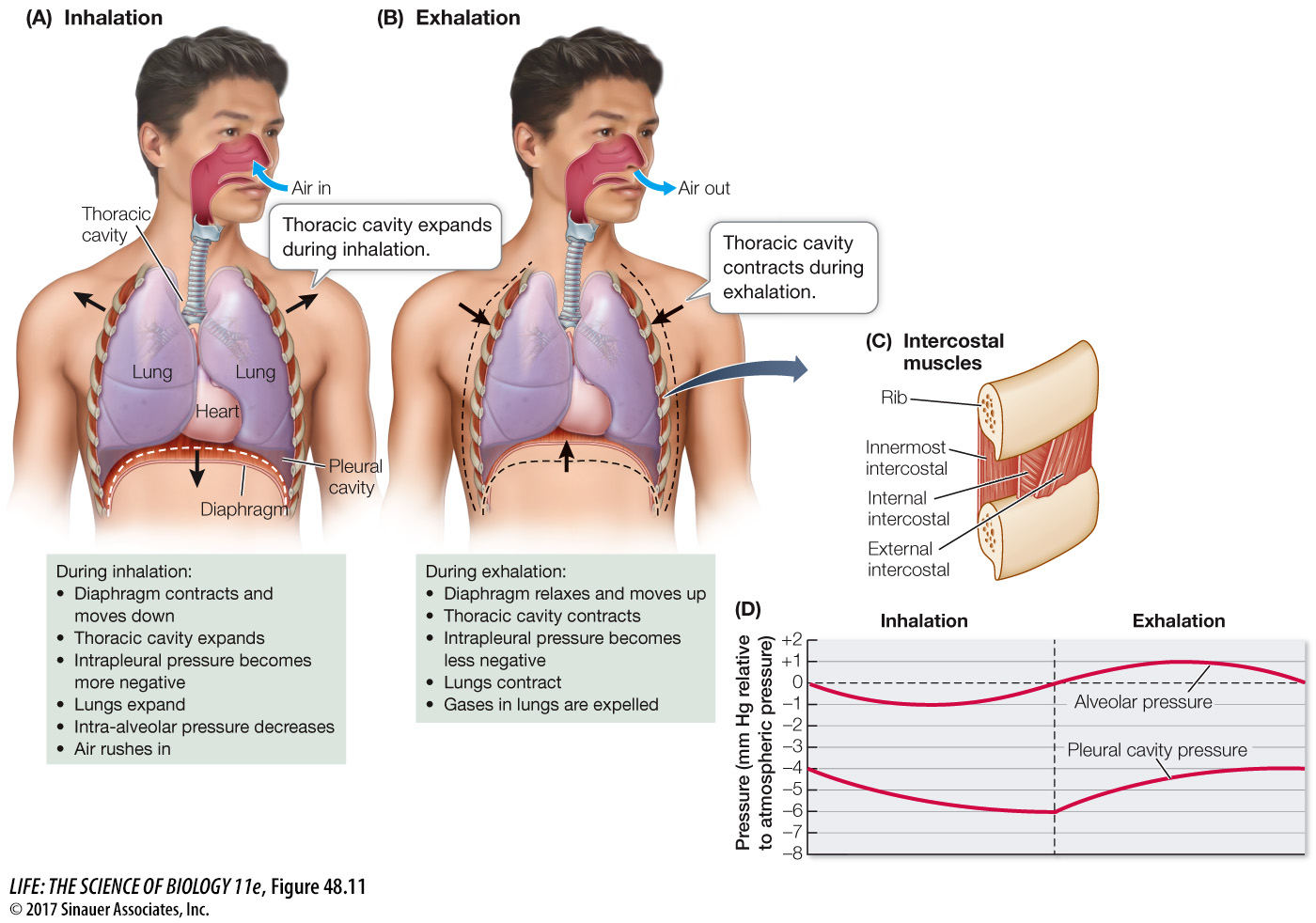
Inhalation and exhalation involve changes in the volume of the thoracic cavity (Figure 48.11). Because the pleural membranes covering the cavity wall and the lung surface are stuck to each other by surface tension, any attempt to increase the volume of the thoracic cavity increases the tension between the pleural membranes. Even between breaths, there is tension between the pleural membranes because the rib cage is pulling outward and the elasticity of the lung tissue is pulling inward. This slight negative pressure keeps the alveoli partly inflated even at the end of an exhalation. If the thoracic cavity is punctured—
Animation 48.2 Airflow in Mammals
www.life11e.com/
1034
At rest, inhalation is initiated by contraction of the muscular diaphragm (see Figure 48.11A). As the domed diaphragm contracts, it pulls down, expanding the thoracic cavity and pulling on the pleural membranes. Since the pleural membranes cannot separate, they pull on the lungs increasing their volume, and air rushes in through the trachea from the outside. Exhalation begins when contraction of the diaphragm ceases. As the diaphragm relaxes, the elastic recoil of the lung tissues pulls the diaphragm up and pushes air out through the airways (see Figure 48.11B). When a person is at rest, inhalation is an active process and exhalation is a passive process.
The diaphragm is not the only muscle that can change the volume of the thoracic cavity. Between the ribs are two sets of intercostal muscles (see Figure 48.11C). The external intercostal muscles expand the thoracic cavity by lifting the ribs up and outward. The internal intercostal muscles decrease the volume of the thoracic cavity by pulling the ribs down and inward. During strenuous exercise, the external intercostal muscles increase the volume of air inhaled, making use of the inspiratory reserve volume, and the internal intercostal muscles increase the amount of air exhaled, making use of the expiratory reserve volume. The abdominal muscles can also aid in breathing. When they contract, they cause the abdominal contents to push up on the diaphragm and thereby contribute to the expiratory reserve volume.
Remember that ventilation and perfusion work together to maximize the partial pressure gradients across the alveolar membranes (see Figure 48.11D). Ventilation delivers O2 to the environmental side of the exchange surface, where it diffuses across and is swept away by the perfusing blood, which carries it to the tissues. The reverse is true for CO2. Perfusion delivers CO2 to the exchange surface, where it diffuses across and is swept away by ventilation.