Arterial pressure is regulated by hormonal and neural mechanisms
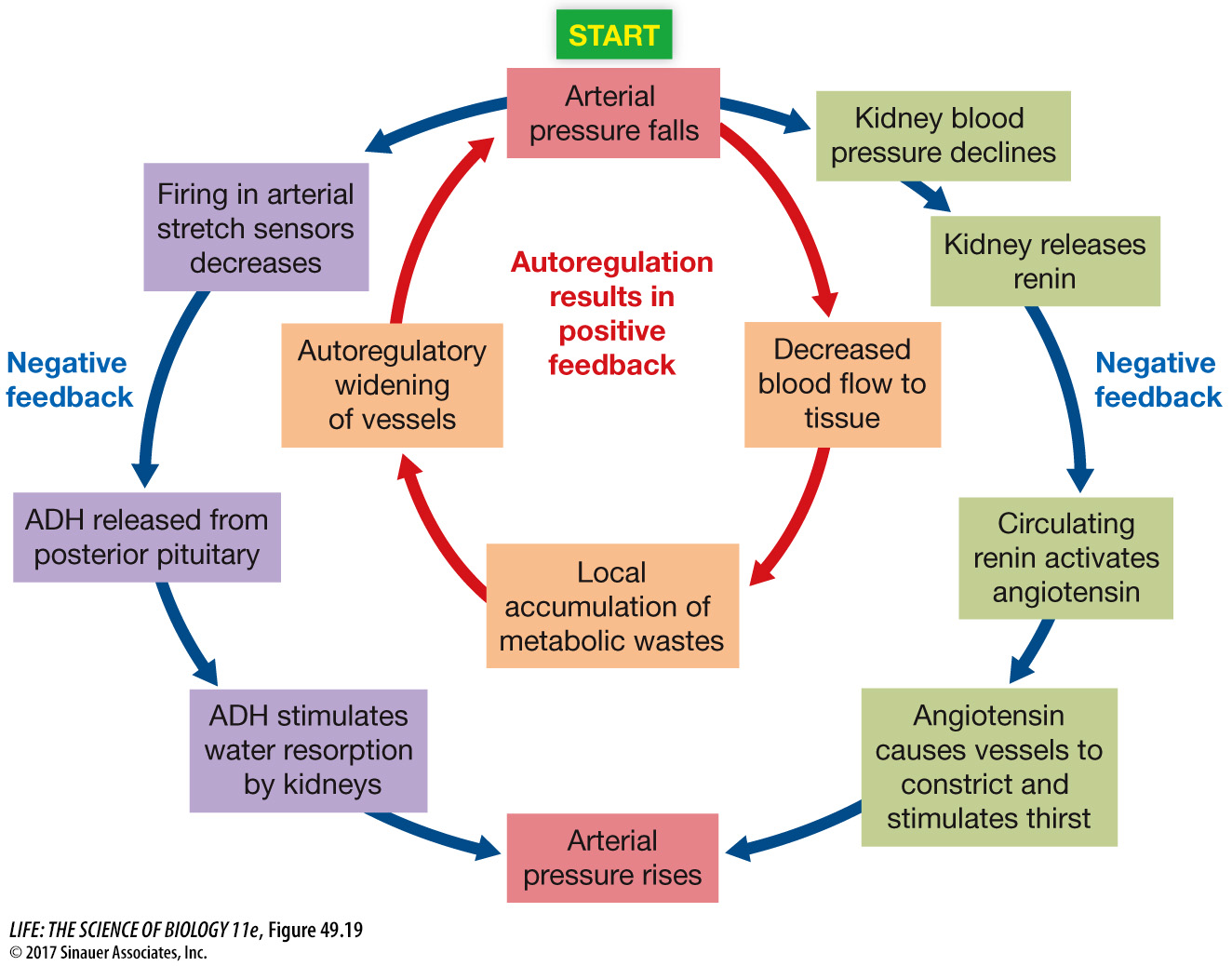
Control and regulation of the circulatory system begins with the local autoregulatory mechanisms that alter the resistance of arteries and arterioles feeding capillary beds. The demands of the capillary beds influence MAP and blood composition. Both of these provide information for the control of endocrine and neural responses that act to return blood pressure and composition to normal. Thus circulatory functions are matched to the regional and overall needs of the body.
1064
Arteries and arterioles are innervated by the autonomic nervous system, particularly the sympathetic division. The sympathetic postganglionic neurotransmitter norepinephrine binds to receptors in smooth muscle in blood vessels in the gut and other tissues not essential for “fight or flight” and causes these vessels to constrict, resulting in reduced blood flow through them and an elevation in MAP. As we discussed earlier in this chapter, increased sympathetic activity increases heart rate, and by increasing the strength of the cardiac muscle contraction, it also increases stroke volume.
Hormones also play a role in regulating arterial pressure. Epinephrine has actions similar to those of norepinephrine and is released from the adrenal medulla during massive sympathetic activation stimulated by a fall in arterial pressure or by activation of the fight-
The autonomic nervous system activity that controls heart rate and constriction of blood vessels originates in a cardiovascular control center in the medulla. Many inputs converge on this central integrative network and influence the commands it issues via parasympathetic and sympathetic nerves (Figure 49.20). Of special importance is incoming information about changes in blood pressure from baroreceptors (stretch receptors) in the walls of the large arteries leading to the brain—
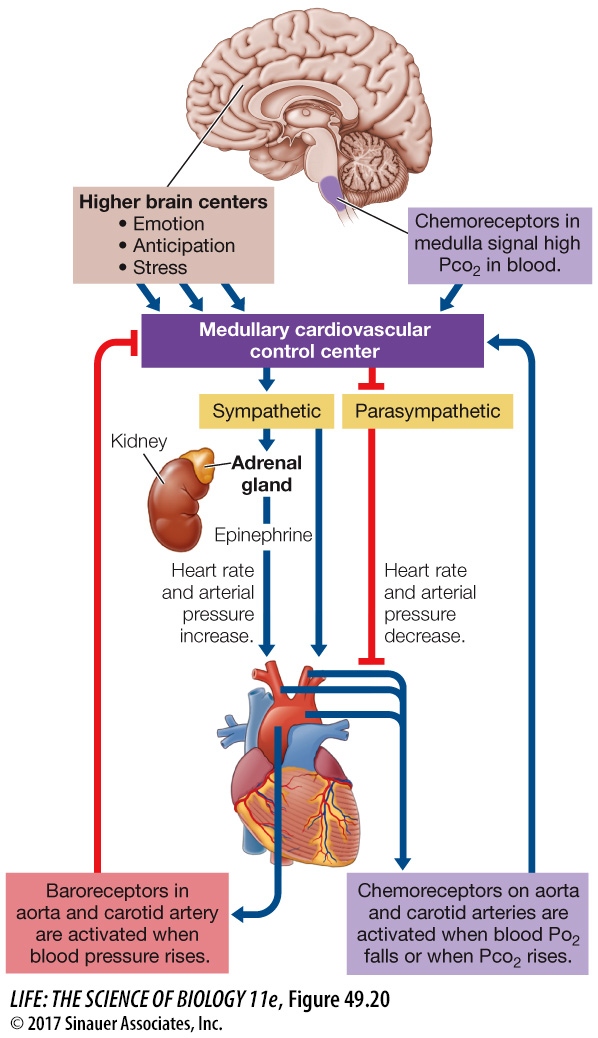
Increased activity in baroreceptors of the large arteries signals rising blood pressure and inhibits sympathetic nervous system signaling to arteries and arterioles while increasing parasympathetic signaling to the heart’s pacemaker. As a result, the heart slows and arterioles in peripheral tissues dilate, reducing blood pressure. If pressure in the large arteries falls, the activity of the baroreceptors decreases, stimulating sympathetic output to the arteries and arterioles while reducing parasympathetic output to the heart’s pacemaker. As a result, the heart beats faster and the arterioles in peripheral tissues constrict, increasing blood pressure.
1065
Another hormone that helps stabilize blood pressure is antidiuretic hormone (ADH), also called vasopressin), which is secreted by the posterior pituitary in response to a fall in the activity of the baroreceptors, signaling a fall in arterial pressure. ADH causes the kidneys to reabsorb more water and thereby maintain blood volume and increase blood pressure (see Figure 51.14). Increased activity of the baroreceptors inhibits the release of ADH, and as a result the kidneys excrete more water, reducing blood volume and contributing to a fall in arterial pressure (see Figure 49.19).
Other information that causes the cardiovascular control center to increase heart rate and blood pressure comes from *chemoreceptors in the medulla, aorta, and the carotid arteries.
*connect the concept Key Concept 48.5 discusses the mechanisms for sensing CO2 and O2 concentrations in the blood. The medullary chemoreceptors are activated by increases in CO2 levels and decreases in pH, and the carotid and aortic bodies are activated by falling O2 levels. Chemoreceptors send signals to the cardiovascular regulatory center as well as to the respiratory regulatory center.