Most chemical digestion occurs in the small intestine
In the small intestine, digestion of carbohydrates and proteins continues, and digestion of fats and absorption of nutrients begin. The small intestine takes its name from its diameter; it is in fact a very large organ, about 6 meters long in an adult human. Given its length and the folds, villi, and microvilli of its epithelial cells, its inner surface area is roughly the size of a tennis court. Across this surface the small intestine absorbs the nutrient molecules derived from food.
The small intestine of humans has three sections. The initial section (about 25 cm long) is called the duodenum and is the site of most digestion; the jejunum and the ileum (together about 600 cm) carry out 90 percent of the absorption of nutrients (see Figure 50.9).
Digestion in the small intestine involves many specialized enzymes, as well as several other secretions. Two accessory organs that are not part of the digestive tract—
LIVER The liver synthesizes bile from cholesterol. Bile also includes other substances, such as phospholipids and bilirubin (the breakdown product of hemoglobin). Bile flows from the liver through the hepatic duct. A side branch off the hepatic duct called the cystic duct goes to the gallbladder, where bile is stored. Below this junction, the hepatic duct is called the common bile duct. Before it reaches the duodenum, the common bile duct is joined by the pancreatic duct (Figure 50.13).
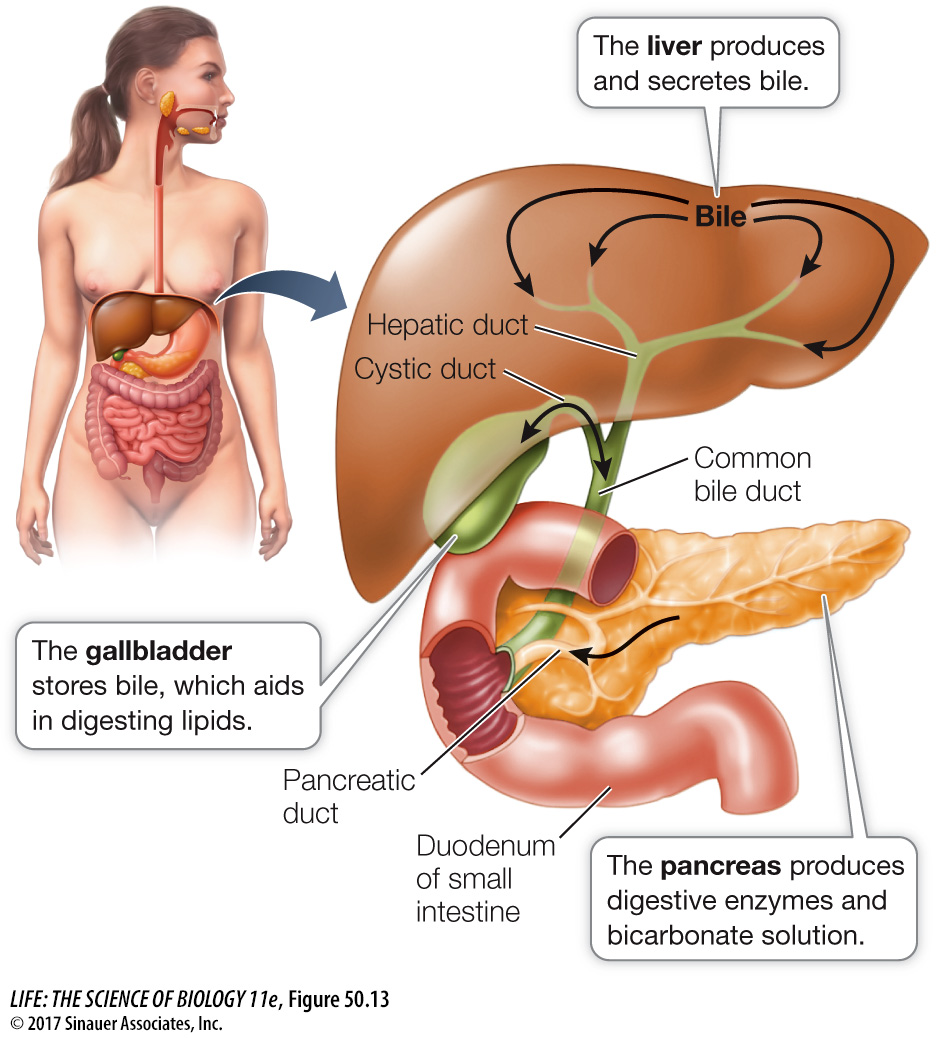
Fat entering the duodenum stimulates cells of the duodenal epithelium to release the hormone cholecystokinin (CCK), which stimulates the walls of the gallbladder to contract rhythmically. As a result, bile is squeezed out of the gallbladder and through the cystic duct to the common bile duct. Peristalsis moves the bile down the bile duct, and a small sphincter at the junction of the common bile duct with the duodenum relaxes in response to waves of peristalsis and allows squirts of bile to enter the duodenal lumen.
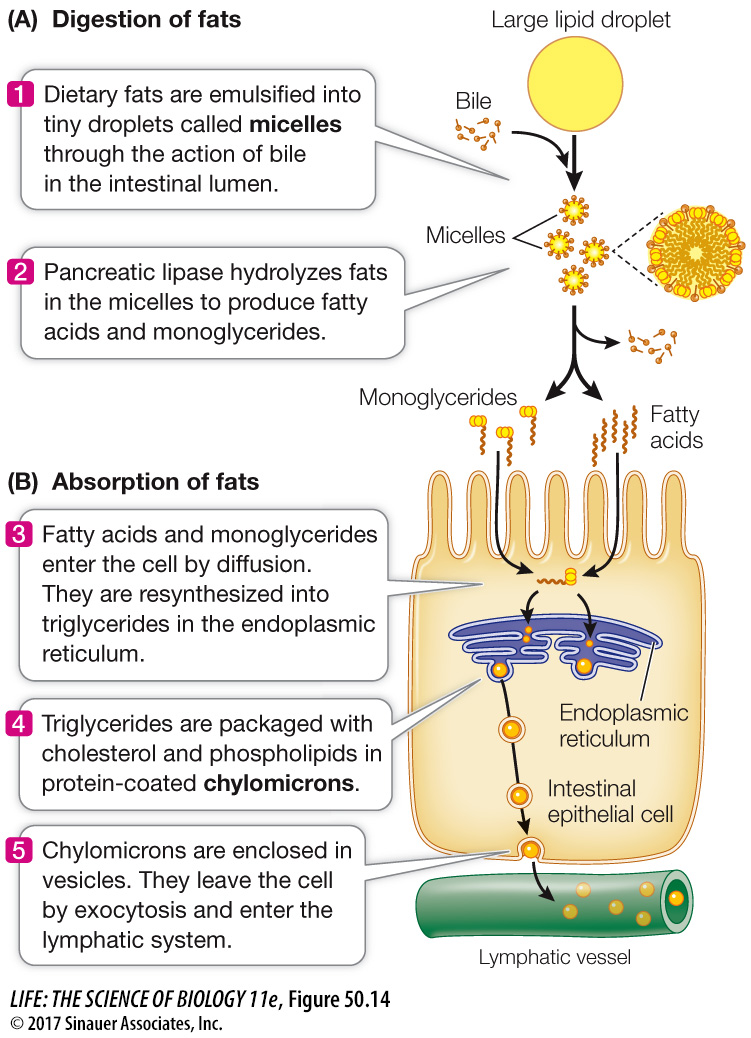
To understand the role of bile in fat digestion, think of an oil-
1083
Question
Q: A small percentage of people who have had their gallbladders removed must thereafter eat a low-
Without a gallbladder, the release of bile into the small intestine is continuous and slow, meaning a large amount of fat passing through cannot be optimally emulsified and digested. As a result it passes through the small intestine without being absorbed and produces fatty stool and diarrhea.
Animation 50.1 The Digestion and Absorption of Fats
www.life11e.com/
PANCREAS The pancreas is a large gland that lies just behind and below the stomach (see Figures 50.9 and 50.13). It is both an endocrine gland (secreting hormones into the circulation; see Key Concept 40.1) and an exocrine gland (secreting digestive juices through the pancreatic duct to the gut lumen). The exocrine tissues of the pancreas produce a host of digestive enzymes, including lipases, amylases, proteases, and nucleases (Table 50.3). As in the stomach, the protease enzymes are released in inactive forms called zymogens; if proteases were not in this inactive state, they would digest the pancreas and its ducts before ever reaching the duodenum. Once in the duodenum, the zymogen trypsinogen is activated by the enzyme enterokinase (secreted by cells lining the duodenum) to produce the active protease trypsin. Trypsin cleaves other zymogens, releasing other proteases as well as more active trypsin.
| Source/enzyme | Action | |
|---|---|---|
| SALIVARY GLANDS | ||
| Salivary amylase | Starch → Maltose | |
| STOMACH | ||
| Pepsin | Proteins → Peptides; autocatalysis | |
| PANCREAS | ||
| Pancreatic amylase | Starch → Maltose | |
| Lipase | Fats → Fatty acids and glycerol | |
| Nuclease | Nucleic acids → Nucleotides | |
| Trypsin | Proteins → Peptides; zymogen activation | |
| Chymotrypsin | Proteins → Peptides | |
| Carboxypeptidase | Peptides → Shorter peptides and amino acids | |
| SMALL INTESTINE | ||
| Aminopeptidase | Peptides → Shorter peptides and amino acids | |
| Dipeptidase | Dipeptides → Amino acids | |
| Enterokinase | Trypsinogen → Trypsin | |
| Nuclease | Nucleic acids → Nucleotides | |
| Maltase | Maltose → Glucose | |
| Lactase | Lactose → Galactose and glucose | |
| Sucrase | Sucrose → Fructose and glucose |
The mixture of zymogens produced by the pancreas can be dangerous if the pancreatic duct is blocked or if the pancreas is injured by infection or physical trauma such as a blow to the abdomen. A few activated trypsin molecules can initiate a chain reaction of enzyme activity that digests the tissues of the pancreas (a condition called pancreatitis), destroying both its endocrine and exocrine functions.
The ducts of the pancreas produce a secretion rich in bicarbonate ions (HCO3–). Bicarbonate ions are alkaline (basic) and neutralize the acidic pH of the chyme that enters the duodenum from the stomach. Intestinal enzymes function best at a neutral or slightly alkaline pH. The production of bicarbonate and its secretion into the pancreatic ducts is similar to the production of H+ ions and their secretion into the gastric pits—