The Medical Revolution
The medical revolution began in the late 1800s with the development of the germ theory of disease (see “Urban Development” in Chapter 24) and continued rapidly after World War II. Scientists discovered vaccines for many of the most deadly diseases. Jonas Salk’s development of the polio vaccine in 1952 was followed by the first oral polio vaccine (1962) and vaccines for measles (1964), mumps (1967), rubella (1970), chicken pox (1974), and hepatitis B (1981). According to the United Nations World Health Organization, medical advances reduced deaths from smallpox, cholera, and plague by more than 95 percent worldwide between 1951 and 1966.
Following independence, Asian and African countries increased the small numbers of hospitals, doctors, and nurses they had inherited from colonial regimes. In addition, local people were successfully trained as paramedics to staff rural outpatient clinics that offered medical treatment, health education, and prenatal and postnatal care. Many paramedics were women, who traditionally addressed health problems that involved childbirth and infancy.
Medical advances significantly lowered death rates and lengthened life expectancies worldwide. Children became increasingly likely to survive their early years, although infant and juvenile mortality remained far higher in poor countries than in rich ones. By 1980 the average inhabitant of the developing countries could expect to live about fifty-four years, although life expectancy at birth varied from forty to sixty-four years depending on the country. In industrialized countries, life expectancy at birth averaged seventy-one years. In 1979 the World Health Organization announced that smallpox had been eradicated worldwide. By this time, surgical transplants of organs such as hearts, lungs, and kidneys had become routine. In 2003 scientists working on the Human Genome Project announced that they had successfully identified, mapped, and sequenced the entire genome, or hereditary genetic information, of human beings, opening new pathways to address illness.
The medical benefits of scientific advances have been limited by unequal access to health care, which is more readily available to the wealthy than to the poor. Between 1980 and 2000 the number of children under the age of five dying annually of diarrhea dropped by 60 percent through the global distribution of a cheap sugar-salt solution mixed in water. Still, over 1.5 million children worldwide continue to die each year from diarrhea, primarily in poorer nations. Deaths worldwide from HIV/AIDS, malaria, and tuberculosis were concentrated in the world’s poorest regions, while tuberculosis remained the leading killer of women worldwide.
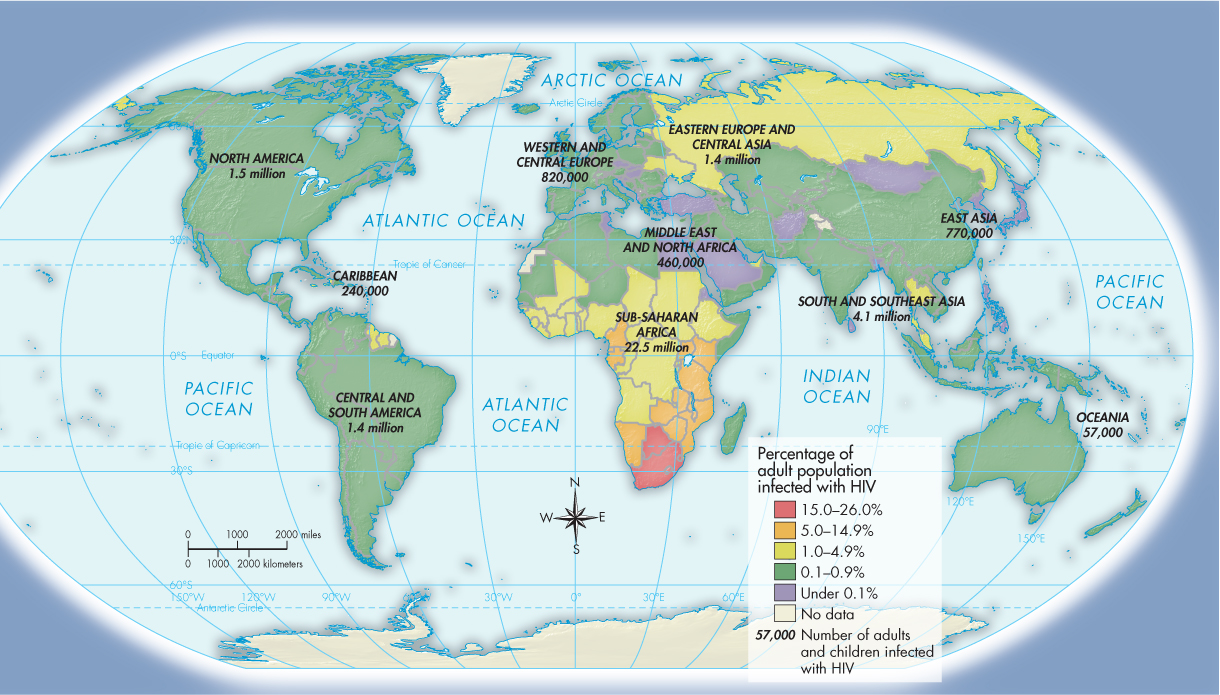
Tuberculosis (TB) claims millions of lives every year, even though it is a curable disease. Malaria kills a million people a year worldwide, 90 percent of them in Africa. In 2007 the Population Division of the United Nations calculated that 36 million persons globally were infected with HIV, the virus that causes AIDS, and that AIDS was the world’s fourth-leading cause of death. About 90 percent of all persons who die from AIDS and 86 percent of those currently infected with HIV live in sub-Saharan Africa (Map 33.3). In Africa HIV/AIDS is most commonly spread through heterosexual sex. Widespread disease and poverty are also significant factors in that Africans already suffering from other illnesses such as malaria or tuberculosis are less resistant to HIV and have less access to health care for treatment.
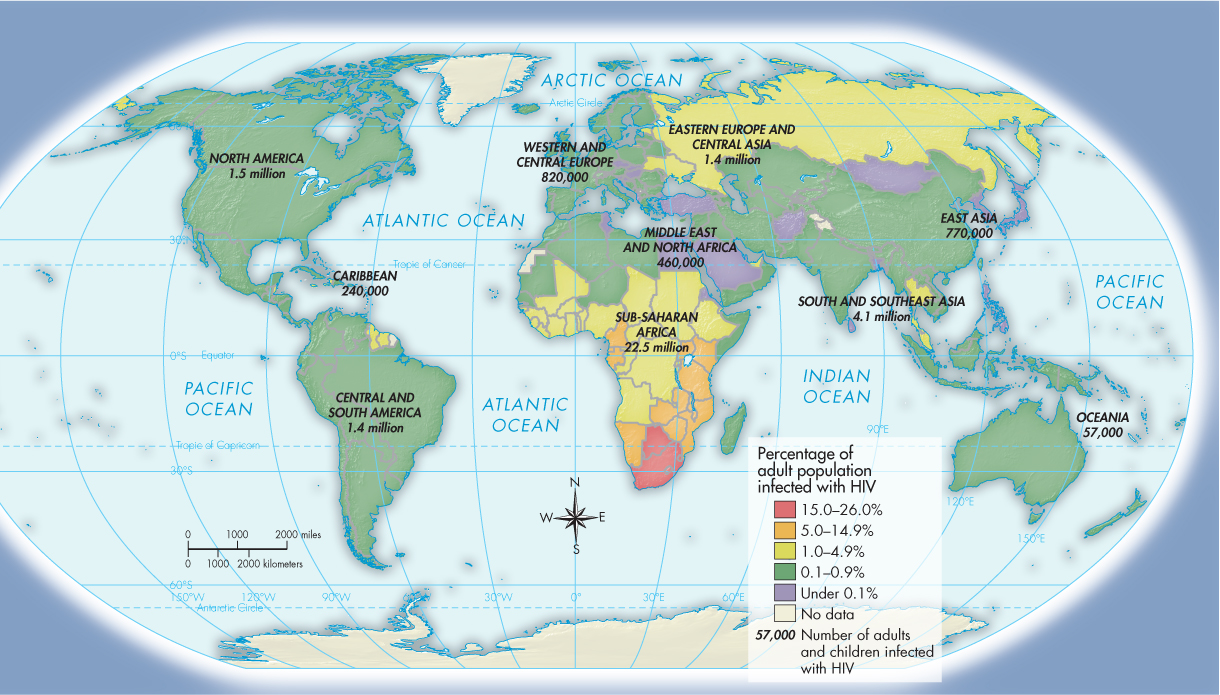
MAP 33.3 People Living with HIV/AIDS Worldwide, ca. 2010 As this map illustrates, Africa has been hit the hardest by the HIV/AIDS epidemic. It currently has fifteen to twenty times more identified cases than any other region of the world. AIDS researchers expect that in the coming decade, however, Russia and South and East Asia will overtake and then far surpass Africa in the number of infected people. (Source: Data from World Health Organization, www.whosea.org)
Another critical factor contributing to the spread of AIDS in Africa is the continued political instability of many countries — particularly those in the corridor running from Uganda to South Africa. This region was the scene of brutal civil and liberation wars that resulted in massive numbers of refugees, a breakdown in basic health-care services, and the destruction of family and cultural networks. The people living in this area in the countries of Uganda, Rwanda, Burundi, Zaire/Congo, Angola, Zimbabwe, Mozambique, and South Africa have been decimated by HIV/AIDS. South Africa currently has the largest number of HIV/AIDS cases in the world. In 2010 around 10 percent of the South African population, about 5.6 million people, were living with HIV/AIDS. Of these, over 330,000 were children under fifteen years of age. An estimated 310,000 South Africans died of AIDS in 2009. Since 2001 relatively inexpensive AIDS drugs that are widely available in the West have been dispensed freely to many of those infected in Africa and Asia, but the availability of these drugs has generally failed to keep up with the need.