Inflammation is a coordinated response to tissue injury.
While there are generally some immune cells already present at the site of tissue injury or infection, many more must be recruited to fight infection successfully. That recruitment happens as part of a process called inflammation. The redness and swelling you see following an injury, a break in the skin, or an infection are signs of inflammation. More precisely, inflammation is a physiological response of the body to injury that removes the inciting agent if present and begins the healing process, such as cell division to heal a wound. It works through the coordinated responses of the local tissue, the vascular system, and the innate immune system. Inflammation is typically beneficial, but if left unchecked or allowed to continue for a long time, it can be debilitating.
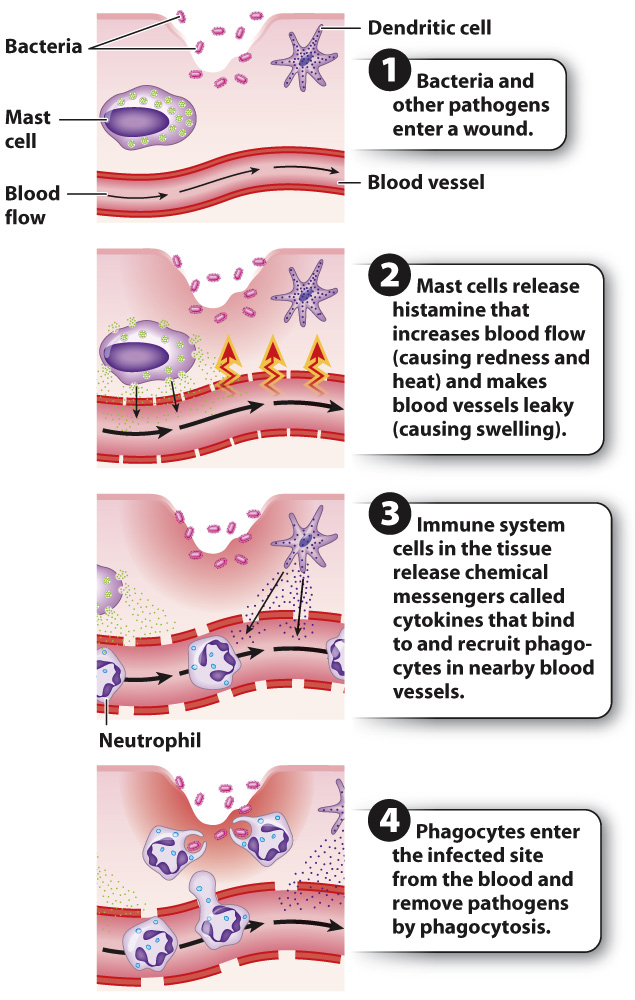
Inflammation is characterized by four signs, described by their Latin names: rubor (redness), calor (heat), dolor (pain), and tumor (swelling). The process begins following tissue injury, such as a cut, or infection, as shown in Fig. 43.5. Certain cells in the tissue, such as dendritic cells and mast cells, recognize a pathogen as foreign and release cytokines and other chemical messengers that recruit more white blood cells to the site or make it easier for them to reach the site quickly. For example, histamine, released by mast cells and basophils, acts directly on blood vessels to cause vasodilation, increasing blood flow to the site of infection or injury. Vasodilation causes the characteristic redness and heat of inflammation. In addition, histamine increases the permeability of the blood vessel wall. Fluid leaks out of the blood vessel, carrying white blood cells into the damaged tissue. The increased fluid in the tissue surrounding the blood vessels is visible as swelling. Some chemical messengers act directly on nerve fibers, causing pain.
927
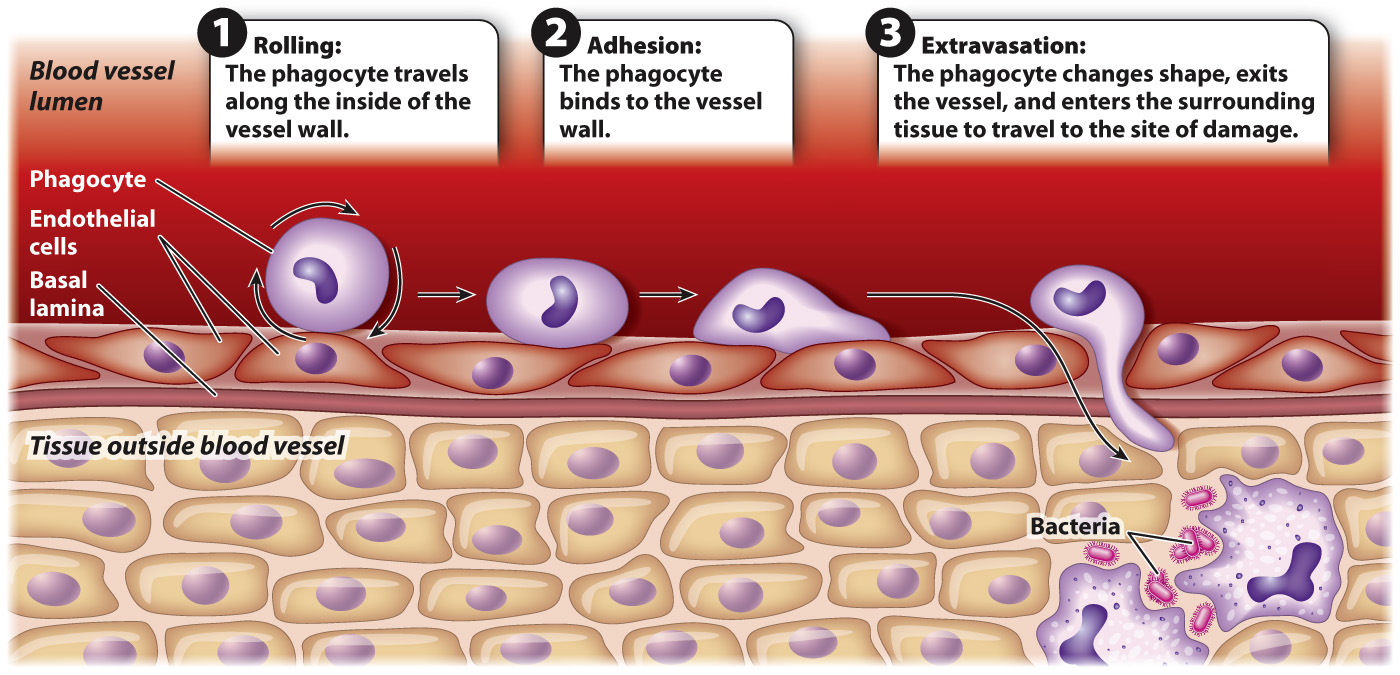
During inflammation, phagocytes in the blood often move from a blood vessel to the site of infection by extravasation (Fig. 43.6). In this process, the phagocyte travels along the vessel wall in a rolling motion, grabbing weakly onto the wall as glycoproteins on the phagocyte surface bind transiently to proteins on the endothelial cells. Stronger interactions put a brake on this rolling motion and allow the phagocyte to adhere more firmly to the vessel wall. As it nears the site of infection, the phagocyte encounters and binds to cytokines. The phagocyte then changes shape and moves in between cells lining the blood vessel and into the surrounding tissue.