The malaria parasite changes surface molecules by antigenic variation.
“Bad air.” That’s the literal translation of “malaria,” a contraction of the Italian mala (“bad”) and aria (“air”). But malaria is not caused by the air. Nor is it caused by a virus or bacterium. Malaria is caused by a single-
Malaria is both devastating and common: There are about 500 million cases and 2 million deaths every year, mostly in sub-
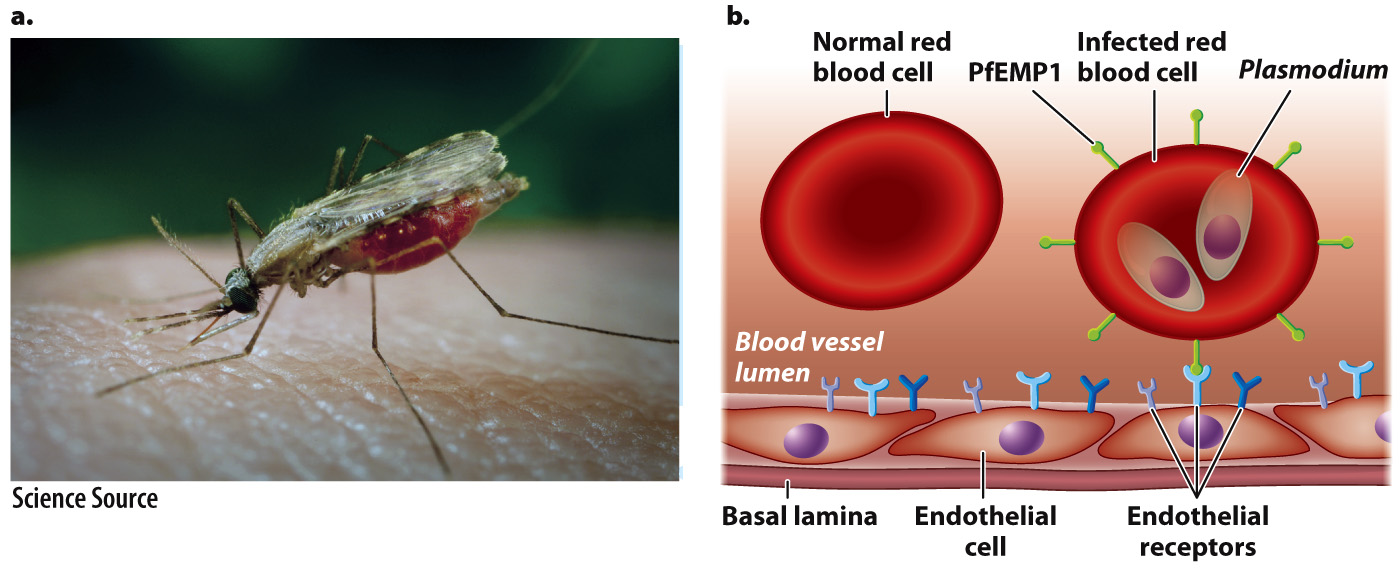
The malaria parasite is transmitted to humans by the bite of an infected mosquito (Fig. 43.20a). Using mosquitoes as a vector, the malaria parasite deftly bypasses the natural protective barrier provided by the skin. The malaria parasite spreads to the liver and then to red blood cells, where it completes its life cycle. The progeny can be taken up again by mosquitoes.
Malaria is an ancient parasite that has coevolved with humans. We have already seen how altered hemoglobin provides some protection against infection (Chapter 21). But the malaria parasite, too, has evolved—
The malaria parasite resides in liver cells and red blood cells. Infected red blood cells can be removed by the spleen, but the malaria parasite has evolved a way to avoid this filtering action. It expresses an adhesive protein, PfEMP1 (Plasmodium falciparum erythrocyte membrane protein 1), that inserts itself on the surface of red blood cells. This protein interacts with proteins on the surface of cells lining blood vessels, helping infected cells stick to blood vessel walls and keeping them in the circulatory system and out of the spleen (Fig. 43.20b). PfEMP1 could conceivably be a target for antibodies or TCRs. However, it is encoded by one of about 60 genes, each slightly different from the others. The parasite expresses just one of these genes at a time and can change which one is expressed, in a process called antigenic variation. The great and ever-
939
Despite continuing research, there is no vaccine. Researchers hope that the sequence of the malaria genome, completed in 2002, will provide new targets for vaccine research. In the meantime, efforts to control malaria focus on measures to control mosquitoes, such as nets and insecticides, and on treatment with antimalarial medications. The evolution of resistance, however, is an all too familiar problem.