Humans have altered the selective landscape for many pathogens.
From the Black Death of the fourteenth century to the flu pandemic of 1918, disease has played a major role in human history. In the Anthropocene Period, we have unprecedented opportunity to control or even eradicate some of the great diseases of the past and present. At the same time, however, the strong selective pressures placed on pathogens by antibiotics pose a key challenge for 21st-
Malaria, discussed in Case 4, provides an illustrative example. In any given year, malaria infects an estimated 500 million people, causing a million or more deaths. Infection is particularly severe in parts of Africa, where the direct and indirect effects of malaria account for almost half of all childhood mortality. Insecticide-
Quinine, a chemical extracted from the bark of the cinchona tree, was the first effective treatment for malaria, and remained in widespread use until the 1940s. Since that time, a small arsenal of antibiotics has been developed, including chloroquine, mefloquine, primaquine, and doxycycline. Their usefulness, however, has declined through time as resistance to each of these drugs has evolved in populations of Plasmodium, the infectious agent of malaria. More recently, artemisinins, antibiotics based on a traditional Chinese plant remedy, have proved effective in treatment. Again, however, resistant strains of malaria have been identified.
1090
Quick Check 5 The interplay of pathogens and antibiotics again brings up the problem of the Red Queen. How does the Red Queen hypothesis apply to these kinds of interaction?
Quick Check 5 Answer
The Red Queen hypothesis suggests that organisms need to keep evolving (running) just to stay in the same ecological niche (place). As new antibiotics are developed, pathogens like malaria frequently evolve resistance, so researchers must continually strive to develop new medicines as natural selection erodes the effectiveness of the old.
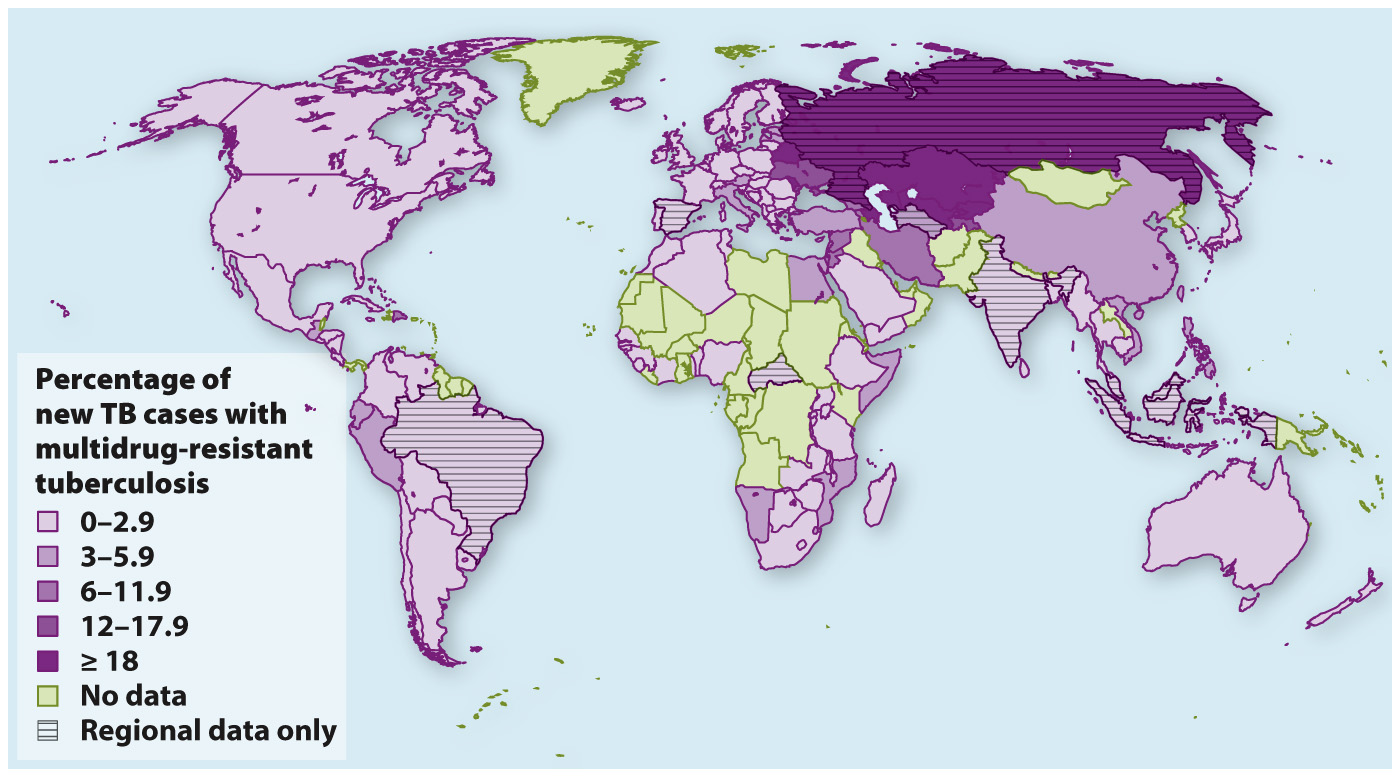
The arms race between antibiotics and pathogens is not limited to malaria. It characterizes nearly the whole range of diseases caused by viruses, bacteria, protists, and fungi that infect humans. For example, tuberculosis, a lung infection spread by inhalation of the bacterium Mycobacterium tuberculosis, causes 1.8 million deaths annually, mostly in sub-
Because bacteria can pass genes horizontally (Chapter 26), antibiotic resistance evolved in one species can jump to another. Thus, the bacterial incubators for drug resistance can arise anywhere and spread rapidly.
Clearly, despite the remarkable gains of the twentieth century, public health will remain a key issue in the decades ahead. Improved sanitation—