34.1 The Physiology of Hunger
34-
Keys’ semistarved volunteers felt their hunger because of a homeostatic system designed to maintain normal body weight and an adequate nutrient supply. But what precisely triggers hunger? Is it the pangs of an empty stomach? So it seemed to A. L. Washburn. Working with Walter Cannon (Cannon & Washburn, 1912), Washburn agreed to swallow a balloon attached to a recording device (FIGURE 34.1). When inflated to fill his stomach, the balloon transmitted his stomach contractions. Washburn supplied information about his feelings of hunger by pressing a key each time he felt a hunger pang. The discovery: Washburn was indeed having stomach contractions whenever he felt hungry.
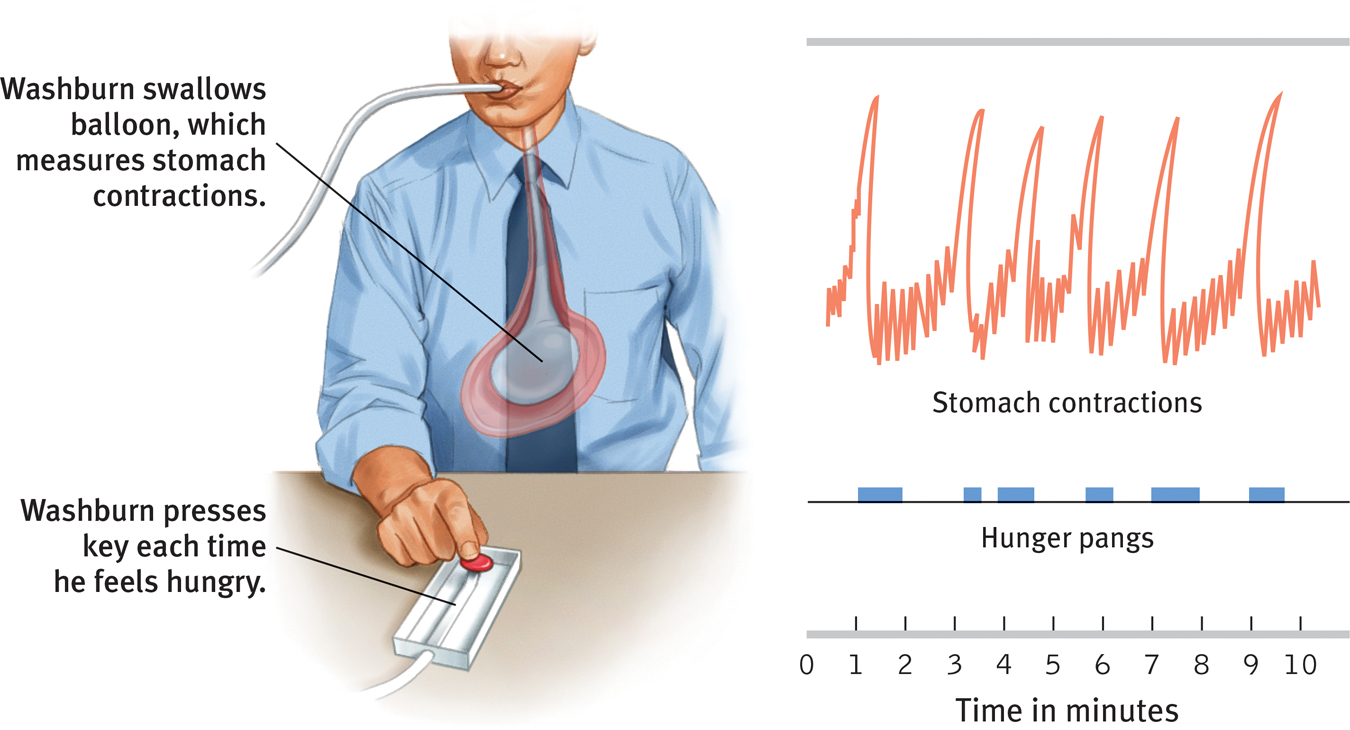
 Figure 34.1
Figure 34.1Monitoring stomach contractions Using this procedure, Washburn showed that stomach contractions (transmitted by the stomach balloon) accompany our feelings of hunger (indicated by a key press). (From Cannon, 1929.)
Can hunger exist without stomach pangs? To answer that question, researchers removed some rats’ stomachs, creating a direct path to their small intestines (Tsang, 1938). Did the rats continue to eat? Indeed they did. Some hunger similarly persists in humans whose ulcerated or cancerous stomachs have been removed.
If the pangs of an empty stomach are not the only source of hunger, what else matters?
Body Chemistry and the Brain
People and other animals automatically regulate their caloric intake to prevent energy deficits and maintain a stable body weight. This suggests that somehow, somewhere, the body is keeping tabs on its available resources. One such resource is the blood sugar glucose. Increases in the hormone insulin (secreted by the pancreas) diminish blood glucose, partly by converting it to stored fat. If your blood glucose level drops, you won’t consciously feel the lower blood sugar. But your brain, which is automatically monitoring your blood chemistry and your body’s internal state, will trigger hunger. Signals from your stomach, intestines, and liver (indicating whether glucose is being deposited or withdrawn) all signal your brain to motivate eating or not.
426
How does the brain integrate these messages and sound the alarm? The work is done by several neural areas, some housed deep in the brain within the hypothalamus, a neural traffic intersection (FIGURE 34.2). For example, one neural arc (called the arcuate nucleus) has a center that secretes appetite-
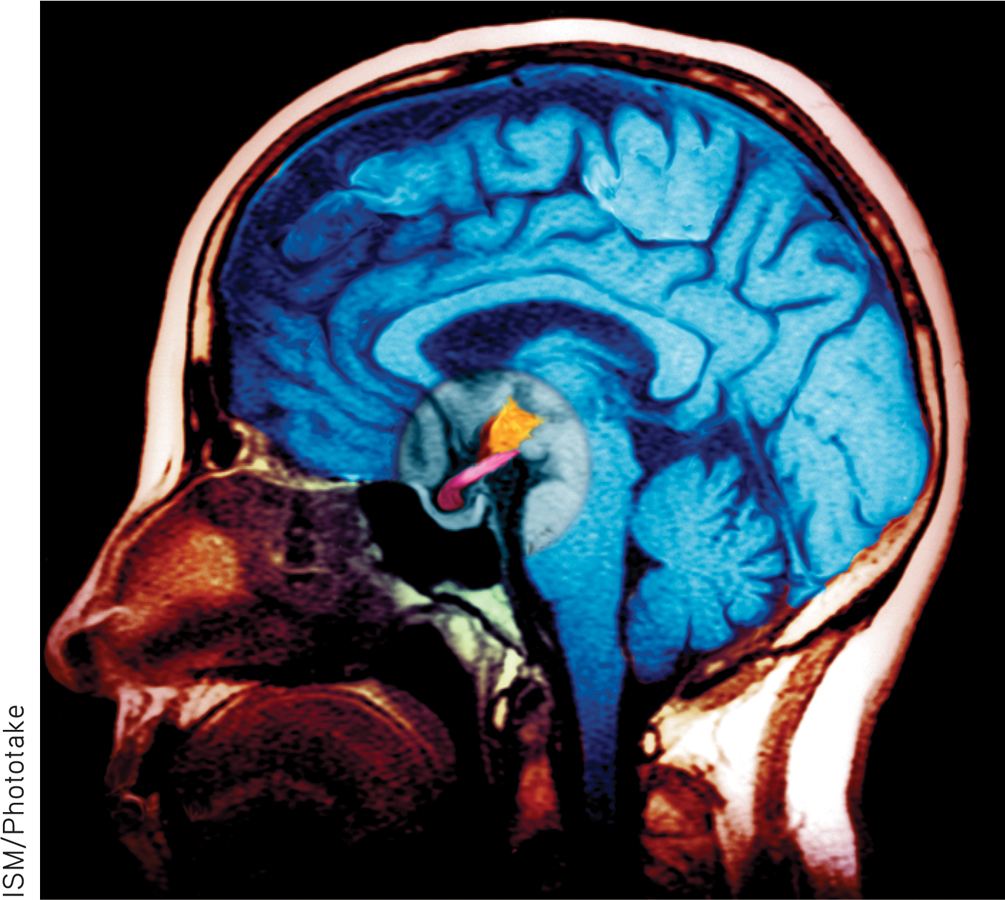
 Figure 34.2
Figure 34.2The hypothalamus The hypothalamus (colored orange) performs various body maintenance functions, including control of hunger. Blood vessels supply the hypothalamus, enabling it to respond to our current blood chemistry as well as to incoming neural information about the body’s state.
Blood vessels connect the hypothalamus to the rest of the body, so it can respond to our current blood chemistry and other incoming information. One of its tasks is monitoring levels of appetite hormones, such as ghrelin, a hunger-
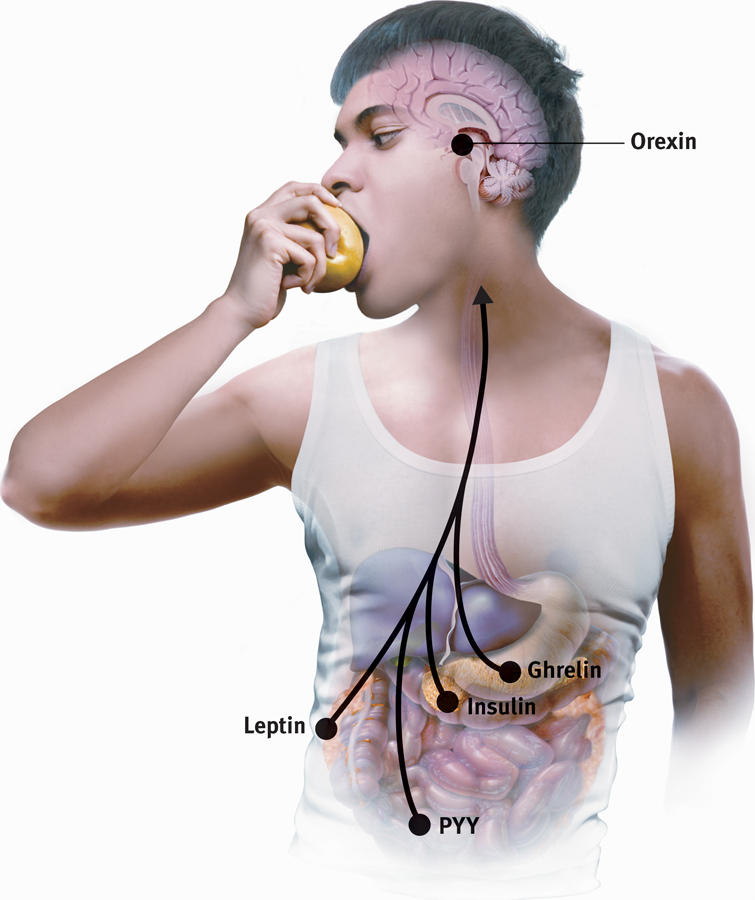
 Figure 34.3
Figure 34.3The appetite hormones
- Ghrelin: Hormone secreted by empty stomach; sends “I’m hungry” signals to the brain.
- Insulin: Hormone secreted by pancreas; controls blood glucose.
- Leptin: Protein hormone secreted by fat cells; when abundant, causes brain to increase metabolism and decrease hunger.
- Orexin: Hunger-triggering hormone secreted by hypothalamus.
- PYY: Digestive tract hormone; sends “I’m not hungry” signals to the brain.
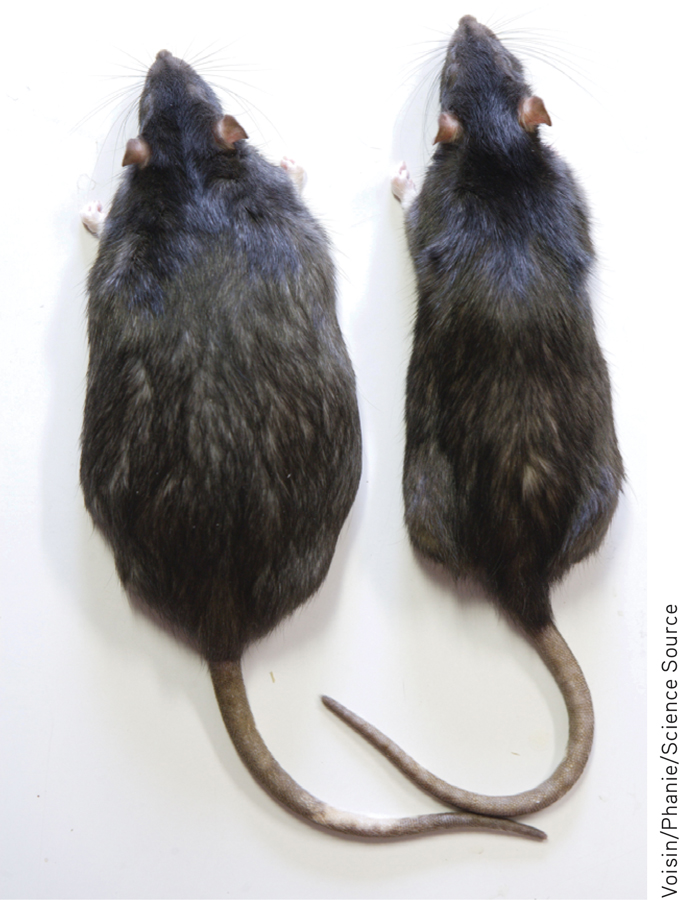
 For an interactive and visual tutorial on the brain and eating, visit LaunchPad’s PsychSim 6: Hunger and the Fat Rat.
For an interactive and visual tutorial on the brain and eating, visit LaunchPad’s PsychSim 6: Hunger and the Fat Rat.
Experimental manipulation of appetite hormones has raised hopes for an appetite-
427
Over the next 40 years you will eat about 20 tons of food. If, during those years, you increase your daily intake by just .01 ounce more than required for your energy needs, you will gain an estimated 24 pounds (Martin et al., 1991).
The complex interaction of appetite hormones and brain activity may help explain the body’s apparent predisposition to maintain itself at a particular weight. When semi-
Our bodies regulate weight through the control of food intake, energy output, and basal metabolic rate—the rate of energy expenditure for maintaining basic body functions when at rest. By the end of their 6 months of semistarvation, the men who participated in Keys’ experiment had stabilized at three-
Some researchers, however, doubt that our bodies have a preset tendency to maintain optimum weight (Assanand et al., 1998). They point out that slow, sustained changes in body weight can alter one’s set point, and that psychological factors also sometimes drive our feelings of hunger. Given unlimited access to a wide variety of tasty foods, people and other animals tend to overeat and gain weight (Raynor & Epstein, 2001). For these reasons, some researchers have abandoned the idea of a biologically fixed set point. They prefer the term settling point to indicate the level at which a person’s weight settles in response to caloric intake and expenditure (which are influenced by environment as well as biology).
RETRIEVAL PRACTICE
- Hunger occurs in response to ____________(low/high) blood glucose and ____________ (low/high) levels of ghrelin.
low; high