23.1 Cancer Is a Group of Diseases Characterized by Cell Proliferation
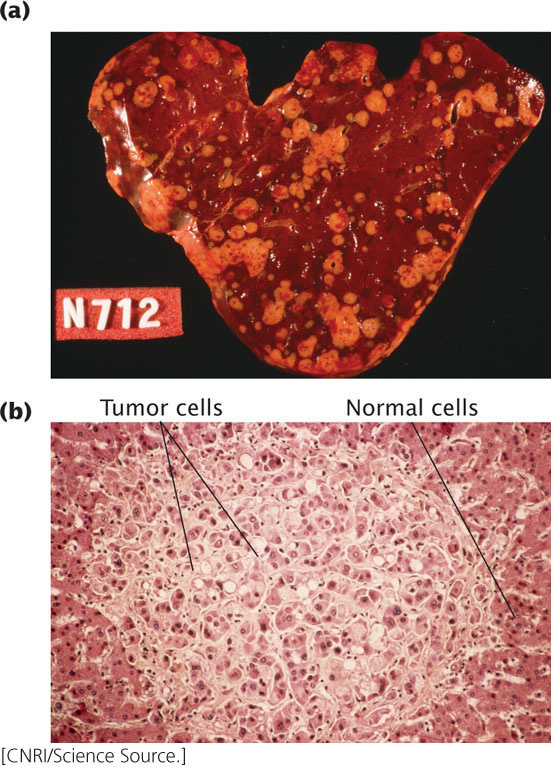
One of every five people in the United States will die from cancer, and cancer treatments cost billions of dollars per year. Cancer is not a single disease; rather, it is a heterogeneous group of disorders characterized by the presence of cells that do not respond to the normal controls on division. Cancer cells divide rapidly and continuously, creating tumors that crowd out normal cells and eventually rob healthy tissues of nutrients (Figure 23.2). The cells of an advanced tumor can separate from the tumor and travel to distant sites in the body, where they may take up residence and develop into new tumors. The most-common cancers in the United States are those of the prostate gland, breast, lung, colon and rectum, and blood (Table 23.1).
| Type of Cancer | New Cases per Year | Deaths per Year |
|---|---|---|
| prostate | 238,590 | 29,720 |
| Breast | 234,580 | 40,030 |
| Lung and bronchus | 228,190 | 159,480 |
| Colon and rectum | 142,820 | 50,830 |
| Lymphoma | 79,030 | 20,200 |
| Melanoma | 76,690 | 9,480 |
| Bladder | 72,570 | 15,210 |
| Uterus | 49,560 | 8,190 |
| Leukemias | 48,610 | 23,720 |
| pancreas | 45,220 | 38,460 |
| Oral cavity and pharynx | 41,380 | 7,890 |
| Liver | 30,640 | 21,670 |
| Brain and nervous system | 23,130 | 14,080 |
| Ovary | 22,240 | 14,030 |
| Stomach | 21,600 | 10,990 |
| Uterine cervix | 12,340 | 4,030 |
| Cancers of soft tissues including heart | 11,410 | 4,390 |
| All cancers | 1,660,290 | 580,350 |
| Source: American Cancer Society, Cancer Facts and Figures, 2013 (Atlanta: American Cancer Society, 2013), p. 4. | ||
Tumor Formation
Normal cells grow, divide, mature, and die in response to a complex set of internal and external signals. A normal cell receives both stimulatory and inhibitory signals, and its growth and division are regulated by a delicate balance between these opposing forces. In a cancer cell, one or more of the signals has been disrupted, which causes the cell to proliferate at an abnormally high rate. As they lose their response to the normal controls, cancer cells gradually lose their regular shape and boundaries, eventually forming a distinct mass of abnormal cells—a tumor. If the tumor cells remain localized, the tumor is said to be benign; if the cells invade other tissues, the tumor is said to be malignant. Cells that travel to other sites in the body, where they establish secondary tumors, have undergone metastasis.
663
Cancer As a Genetic Disease
Cancer arises as a result of fundamental defects in the regulation of cell division, and its study therefore has significance not only for public health, but also for our basic understanding of cell biology. Through the years, many ideas have been put forth to explain cancer, but we now recognize that most, if not all, cancers arise from defects in DNA.
Genetic Evidence for Cancer
Early observations suggested that cancer might result from genetic damage. First, many agents, such as ionizing radiation and chemicals, that cause mutations also cause cancer (are carcinogens, see Chapter 18). Second, some cancers are consistently associated with particular chromosome abnormalities. About 90% of people with chronic myeloid leukemia, for example, have a reciprocal translocation between chromosome 22 and chromosome 9. Third, some specific types of cancers tend to run in families. Retinoblastoma, a rare childhood cancer of the retina, appears with high frequency in a few families and is inherited as an autosomal dominant trait, suggesting that a single gene is responsible for these cases of the disease.
Although these observations hinted that genes play some role in cancer, the theory of cancer as a genetic disease had several significant problems. If cancer is inherited, every cell in the body should receive the cancer-causing gene and therefore every cell should become cancerous. In the types of cancer that run in families, however, tumors typically appear only in certain tissues and often only when the person reaches an advanced age. Finally, many cancers do not run in families at all and, even in regard to those cancers that generally do, isolated cases crop up in families with no history of the disease.
Knudson’s Multistep Model of Cancer
In 1971, Alfred Knudson proposed a model to explain the genetic basis of cancer. Knudson was studying retinoblastoma, which usually develops in only one eye but occasionally appears in both. Knudson found that, when retinoblastoma appears in both eyes, onset is at an early age, and affected children often have close relatives who also have the disease.
Knudson proposed that retinoblastoma results from two separate genetic defects, both of which are necessary for cancer to develop (Figure 23.3). He suggested that, in the cases in which the disease affects just one eye, a single cell in one eye undergoes two successive mutations. Because the chance of these two mutations occurring in a single cell is remote, retinoblastoma is rare and typically develops in only one eye. For the bilateral case, Knudson proposed that the child inherited one of the two mutations required for the cancer, and so every cell contains this initial mutation. In these cases, all that is required for cancer to develop is for one eye cell to undergo the second mutation. Because each eye possesses millions of cells, the probability that the second mutation will occur in at least one cell of each eye is high, producing tumors in both eyes at an early age.
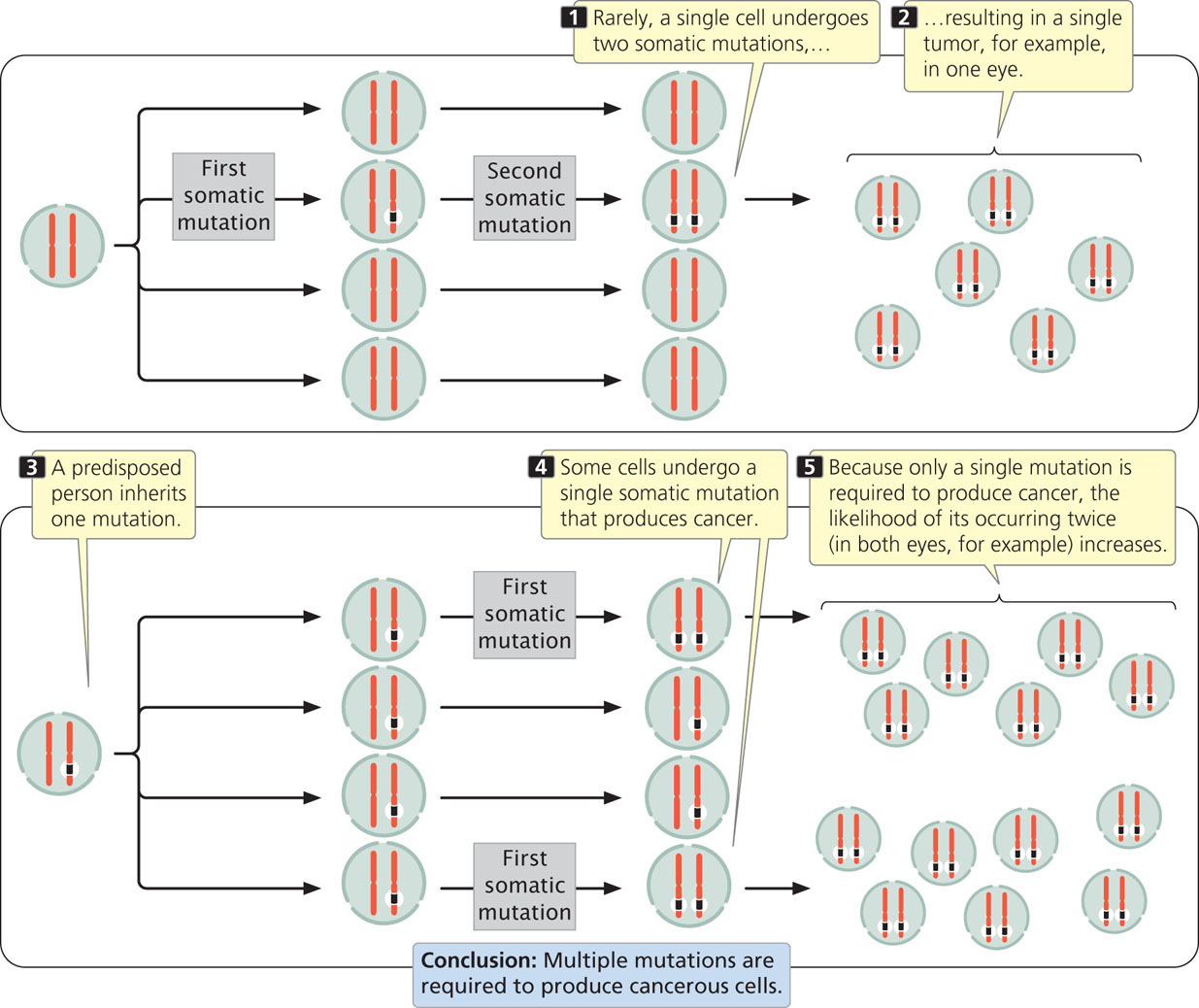
Knudson’s proposal suggests that cancer is the result of a multistep process that requires several mutations. If one or more of the required mutations is inherited, fewer additional mutations are required to produce cancer, and the cancer will tend to run in families. Knudson’s idea has been called the “two-hit hypothesis” because, for retinoblastoma, only two mutations are necessary to cause a tumor. However, for most cancers more than two mutations are involved in the transformation of normal cells into cancer cells. In the case of retinoblastoma, the two required mutations occur at the same locus (both alleles become mutated), but for many cancers mutations at different loci are required for the development of cancer. The idea that cancer results from multiple mutations turns out to be correct for most cancers.
Knudson’s genetic theory for cancer has been confirmed by the identification of genes that, when mutated, cause cancer. Today, we recognize that cancer is fundamentally a genetic disease, although few cancers are actually inherited. Most tumors arise from somatic mutations that accumulate in a person’s life span, either through spontaneous mutation or in response to environmental mutagens.  TRY PROBLEM 24
TRY PROBLEM 24
664
The Clonal Evolution of Tumors
Cancer begins when a single cell undergoes a mutation that causes the cell to divide at an abnormally rapid rate. The cell proliferates, giving rise to a clone of cells, each of which carries the same mutation. Because the cells of the clone divide more rapidly than normal, they soon outgrow other cells. An additional mutation that arises in some of the clone’s cells may further enhance the ability of those cells to proliferate, and cells carrying both mutations soon become the most-common cells in the clone. Eventually, they may be overtaken by cells that contain yet more mutations that enhance proliferation. In this process, called clonal evolution, the tumor cells acquire more mutations that allow them to become increasingly more aggressive in their proliferative properties (Figure 23.4).
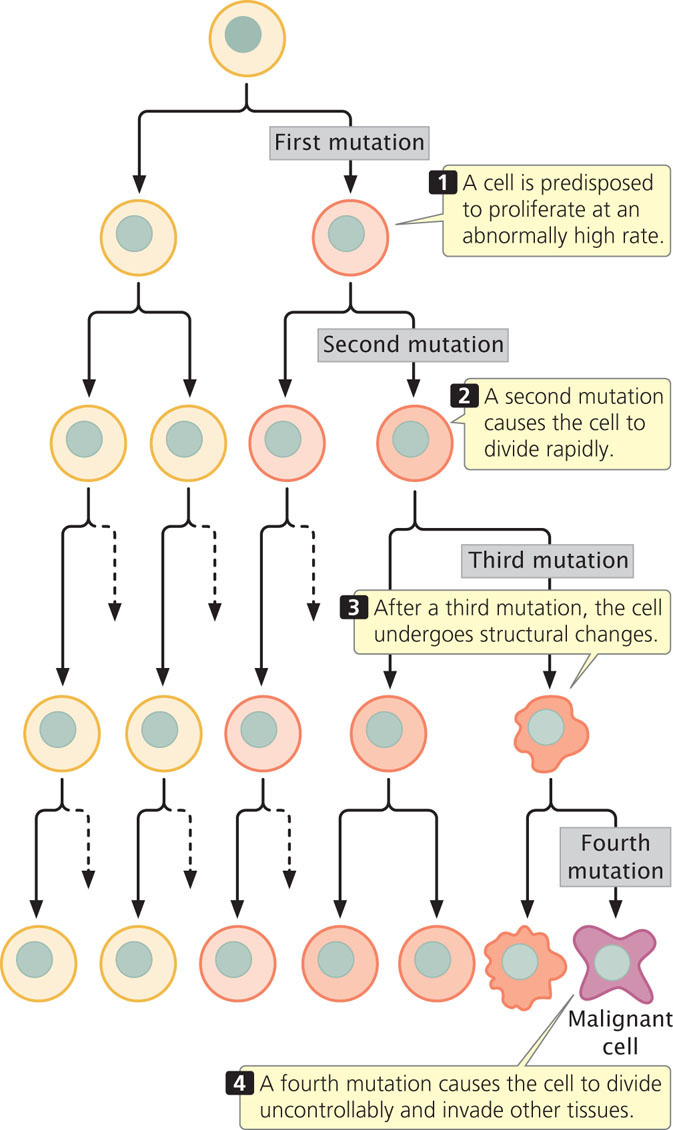
The rate of clonal evolution depends on the frequency with which new mutations arise. Any genetic defect that allows more mutations to arise will accelerate cancer progression. Genes that regulate DNA repair are often found to have been mutated in the cells of advanced cancers, and inherited disorders of DNA repair are usually characterized by increased incidences of cancer. Because DNA-repair mechanisms normally eliminate many of the mutations that arise, cells with defective DNA-repair systems are more likely to retain mutations than are normal cells, including mutations in genes that regulate cell division. Xeroderma pigmentosum, for example, is a rare disorder caused by a defect in DNA repair (see Chapter 18). People with this condition have elevated rates of skin cancer when exposed to sunlight (which induces mutation). Similarly, breast cancer can be caused by mutations in BRCA1 and BRCA2, two genes that function in DNA repair.
Mutations in genes that affect chromosome segregation also may contribute to the clonal evolution of tumors. Many cancer cells are aneuploid (contain extra or missing copies of individual chromosomes, see Chapter 8) and, clearly, chromosome mutations contribute to cancer progression by duplicating some genes (those on extra chromosomes) and eliminating others (those on deleted chromosomes). Cellular defects that interfere with chromosome separation increase aneuploidy and may therefore accelerate cancer progression.
665
CONCEPTS
Cancer is fundamentally a genetic disease. Mutations in several genes are usually required to produce cancer. If one of these mutations is inherited, fewer somatic mutations are necessary for cancer to develop, and the person may have a predisposition to cancer. Clonal evolution is the accumulation of mutations in a clone of cells.
 CONCEPT CHECK 1
CONCEPT CHECK 1
How does the multistep model of cancer explain the observation that sporadic cases of retinoblastoma usually appear in only one eye, whereas inherited forms of the cancer appear in both eyes?
The Role of Environmental Factors in Cancer
Although cancer is a genetic disease, most cancers are not inherited, and many are influenced by environmental factors. The role of environmental factors in cancer is suggested by differences in the incidence of specific cancers throughout the world (Table 23.2). The results of studies show that migrant populations typically take on the cancer incidence of their host country. For example, the overall rates of cancer are considerably lower in Japan than in Hawaii. However, within a single generation after migration to Hawaii, Japanese people develop cancer at rates similar to those of native Hawaiians. The increased cancer among the migrants is due to the fact that they are exposed to the same environmental factors as are the natives.
| Type of Cancer | Location | Incidence Rate* |
|---|---|---|
| Lip | Canada (Newfoundland) | 15.1 |
| Brazil (Fortaleza) | 1.2 | |
| Nasopharynx | Hong Kong | 30.0 |
| United States (Utah) | 0.5 | |
| Colon | United States (Iowa) | 30.1 |
| India (Mumbai) | 3.4 | |
| Lung | United States (New Orleans, African Americans) | 110.0 |
| Costa Rica | 17.8 | |
| Prostate | United States (Utah) | 70.2 |
| China (Shanghai) | 1.8 | |
| Bladder | United States (Connecticut, Whites) | 25.2 |
| Philippines (Rizal) | 2.8 | |
| All cancer | Switzerland (Basel) | 383.3 |
| Kuwait | 76.3 | |
| Source: C. Muir et al., Cancer Incidence in Five Continents, vol. 5 (Lyon: International Agency for Research on Cancer, 1987), Table 12-2. | ||
| * The incidence rate is the age-standardized rate in males per 100,000 population. | ||
A number of environmental factors contribute to cancer, but those that have the greatest effects include tobacco use, diet, obesity, alcohol, and UV radiation (Table 23.3). Other environmental factors that induce cancer are certain types of chemicals, such as benzene (used as an industrial solvent), benzo[a]pyrene (found in cigarette smoke), and polychlorinated biphenyls (PCBs; used in industrial transformers and capacitors). Most environmental factors associated with cancer cause somatic mutations that stimulate cell division or otherwise affect the process of cancer progression.
| Factor | Percentage of Cancer Cases |
|---|---|
| Tobacco | 19.4 |
| Diet | 9.2 |
| Overweight and obesity | 5.5 |
| Alcohol | 4.0 |
| Occupation | 3.7 |
| Radiation (UV) | 3.5 |
| Infections | 3.1 |
| Radiation (ionizing) | 1.8 |
| All environmental factors | 42.7 |
| Source: Parkin, D.M., L. Boyd, and L.C. Walker. 2011. Fraction of cancer attributable to lifestyle and environmental factors in the UK in 2010. British Journal of Cancer 105:S77-S81. | |
Environmental factors may interact with genetic predispositions to cancer. For example, lung cancer is clearly associated with smoking, an environmental factor. Genomewide association studies (see Chapter 20) revealed that variation at several genes predisposes some people to smoking-induced lung cancer. Variants at some of these genes cause people to be more likely to become addicted to smoking. Other predisposing genes encode receptors that bind potential carcinogens in cigarette smoke.  TRY PROBLEM 23
TRY PROBLEM 23
666