DIABETES TREATMENT AND PREVENTION
People with type 1 diabetes must receive injections of insulin to manage their blood glucose levels. An insulin pill isn’t yet on the horizon—
109


RESISTANT STARCH a starch that remains intact after cooking, is not broken down by human digestive enzymes, and is not absorbed from the intestines
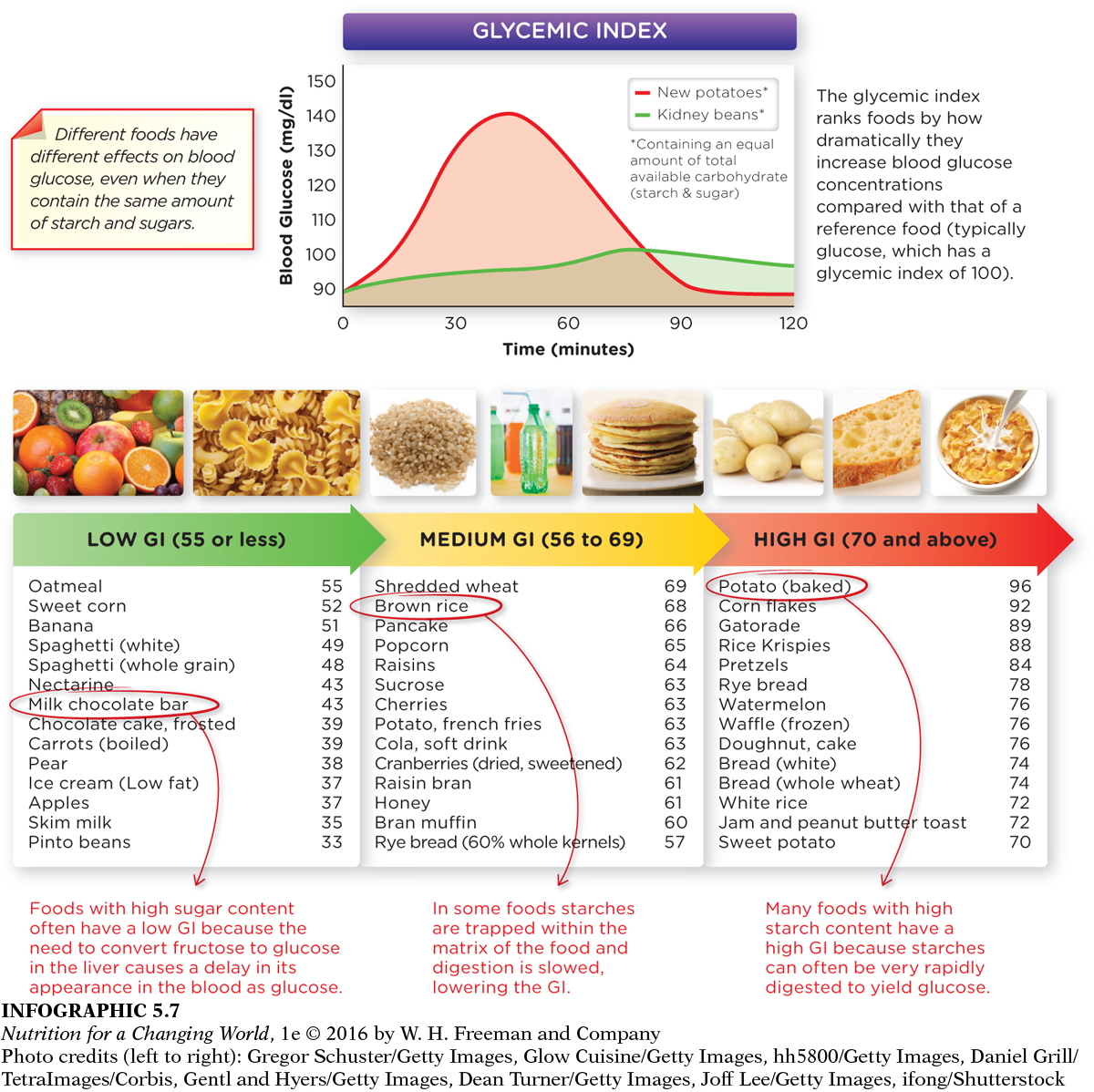
Different foods have different effects on blood glucose, even when they contain the same amount of starch and sugars. Specifically, how the body processes particular carbohydrates dictates how much and at what rate glucose will be released into the bloodstream and therefore how much insulin is released. For example, starches in foods can be partially “trapped” within the physical structure of grains or in the internal portion of larger food particles. These physical structures can make it difficult for digestive enzymes to gain access to the starch, slowing digestion and the subsequent appearance of glucose in blood. Such starches, that remain undigested and enter the large intestine, are called resistant starches. Diets high in resistant starch may improve insulin sensitivity and make people feel full for longer periods. Examples of foods high in resistant starches include beans, under-
110

At the other extreme, starches in some foods—
Surprisingly, sucrose, lactose, and fructose and foods that contain these sugars (such as candies, dairy foods, or fruit) often produce a less dramatic rise in blood glucose than starchy foods. This is because fructose and galactose (a monosaccharide in lactose) have no immediate impact on blood glucose levels, until they are converted to glucose in the liver. Diets high in fiber, especially soluble fiber, also seem to help control blood glucose levels. One study found that people who consumed 50 grams of fiber per day with at least half as soluble fiber were able to control their blood glucose better than those who ate less fiber.
GLYCEMIC INDEX a number used to rank carbohydrate foods by their ability to raise blood glucose levels compared with a reference standard
Since food sources of carbohydrates have different effects on blood glucose levels, Laffel tells children and their families to pay attention to a measure known as glycemic index (GI) which ranks foods by how quickly and to what degree they raise blood glucose levels. The amount of available carbohydrate (starch and sugars) present in the food is compared with the equivalent amount of glucose, which has a GI of 100. Foods with a high GI raise blood glucose quickly and cause considerable spikes in blood glucose levels, while foods with a low GI cause a smaller and more gradual increase. Low GI diets help individuals with diabetes better control blood glucose levels and are associated with reduced risk of developing type 2 diabetes.
Although glycemic index can be a helpful measure to consider, it has some limitations. For example, we rarely eat carbohydrate containing foods in consistently the same amounts (smaller or larger amounts would alter the GI) or eat these foods by themselves. And even carbs with high GIs have less effect on blood glucose when consumed with protein, fat, or fiber, which all delay gastric emptying. Even factors such as the ripeness of a fruit or how a carbohydrate is processed can alter its GI. (INFOGRAPHIC 5.7)
111
Question 5.7
 What are two additional foods that are high in starch and have a high GI, and two additional foods that are high in sugar and have a low GI?
What are two additional foods that are high in starch and have a high GI, and two additional foods that are high in sugar and have a low GI?
Foods with high GIs and starch include graham crackers and soda crackers. Foods with high sugar and low GI include cherries and dark chocolate.
GLYCEMIC LOAD the extent of increase in blood glucose levels, calculated by multiplying glycemic index by the carbohydrate content of a food
The GI of a food, however, often does not reflect the amount of carbohydrates contained in the servings of food that we typically consume. Foods with a low to moderate GI can still cause a dramatic rise in blood glucose levels if consumed in large amounts. So consumers can also consult the glycemic load (GL), which calculates the effect of the actual serving size of food on blood glucose (by multiplying the GI by a food’s grams of carbohydrates, divided by 100). The GL is a more useful assessment of a food’s effect on blood glucose.
Some research suggests that diets emphasizing low-
CARBOHYDRATE COUNTING a method to track carbohydrates consumed so that those with diabetes can appropriately balance physical activity and medication to manage blood glucose levels
Registered dietitians and other health care providers may also teach their patients with diabetes about carbohydrate counting, or “carb counting,” a meal-
112
Physical activity also helps improve insulin sensitivity, lower blood glucose levels, and keep weight off over the long term. Exercise alone may not be enough—
When those lifestyle changes aren’t enough, oral medications are available to lower blood glucose levels of individuals with type 2 diabetes, and some people may require insulin injections to get their glucose under control.

Hypoglycemia
HYPOGLYCEMIA abnormally low blood glucose levels, resulting in symptoms of anxiety, hunger, sweating, and heart palpitations (fasting plasma glucose < 70 mg/dl)
It is possible to overmedicate patients with diabetes; they can develop hypoglycemia, in which their blood glucose levels drop too low (diagnosed when < 70mg/100 ml blood), causing symptoms ranging from irritability, headache, hunger, weakness or fatigue, sweating, and rapid heartbeat.
EPINEPHRINE (ADRENALINE) a hormone released from the adrenal glands to help the body prepare for a fight-
There are different types of hypoglycemia—
■ ■ ■
Today, millions of people take insulin and, along with appropriate diet and physical activity, are able to manage their diabetes and lead productive, healthy, and happy lives.
Although the work of Banting and his colleagues to develop insulin revolutionized diabetes therapy, scientists are continuing to investigate ways to treat diabetes without relying on cumbersome and unpleasant injections—
113
Research toward a cure for type 1 diabetes is ongoing and varied in approach. Efforts have been made to understand the immune system attack that causes type 1 diabetes, and to intervene in that process. Another important effort is to regenerate the cells that produce insulin through the use of embryonic or adult stem cells.
While the development of insulin therapy revolutionized diabetes treatment, today we face an increasing epidemic of type 2 diabetes and concern about the long-