STOCKPILING THE ANTIBIOTIC ARSENAL
GRAM-POSITIVE Refers to bacteria with a cell wall that includes a thick layer of peptidoglycan that retains the Gram stain.
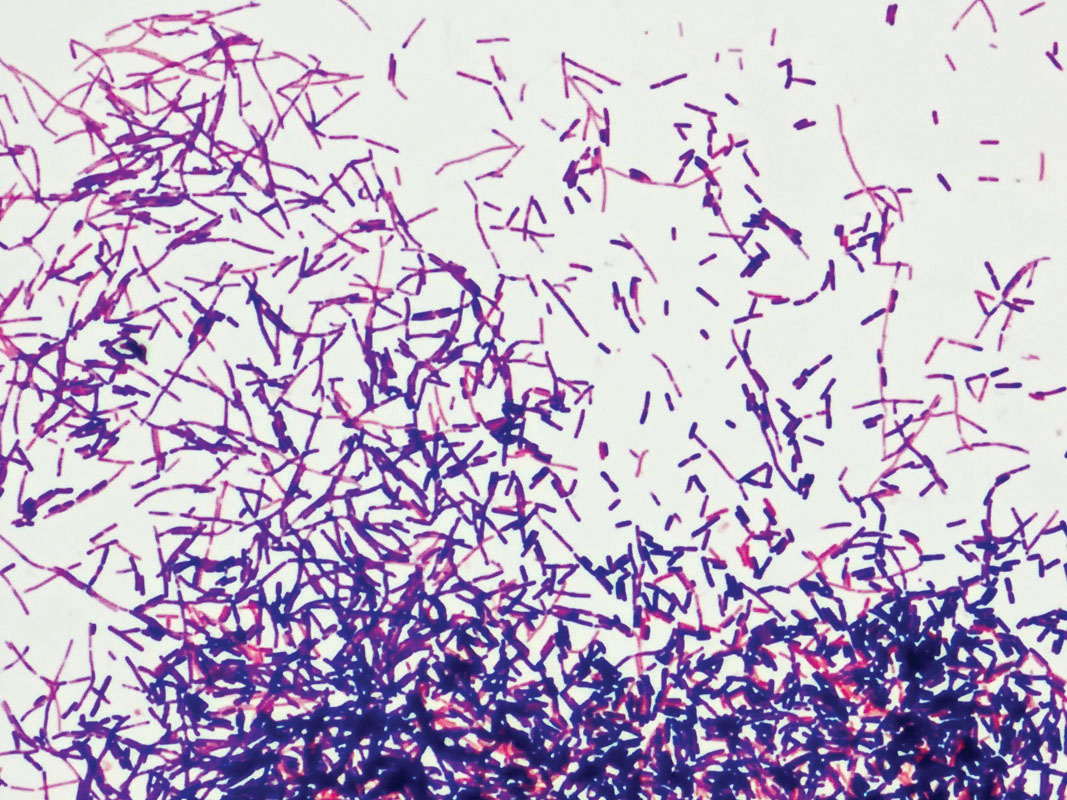
As Fleming knew, most of the bacterial world falls into one of two categories, Gram-positive or Gram-negative; these names reflect the way bacterial cell walls trap a dye known as Gram stain (after its discoverer, the Danish scientist Hans Christian Gram). Fleming found that while penicillin easily killed Gram-positive bacteria like Staphylococcus and Streptococcus, the microbes that cause staph infections and strep throat, respectively, it had little effect on Gram-negative bacteria like Escherichia coli and Salmonella, whose cell walls have an extra layer of lipids surrounding them. This extra lipid layer prevents penicillin from reaching the peptidoglycan underneath.
GRAM-NEGATIVE Refers to bacteria with a cell wall that includes a thin layer of peptidoglycan surrounded by an outer lipid membrane that does not retain the Gram stain.
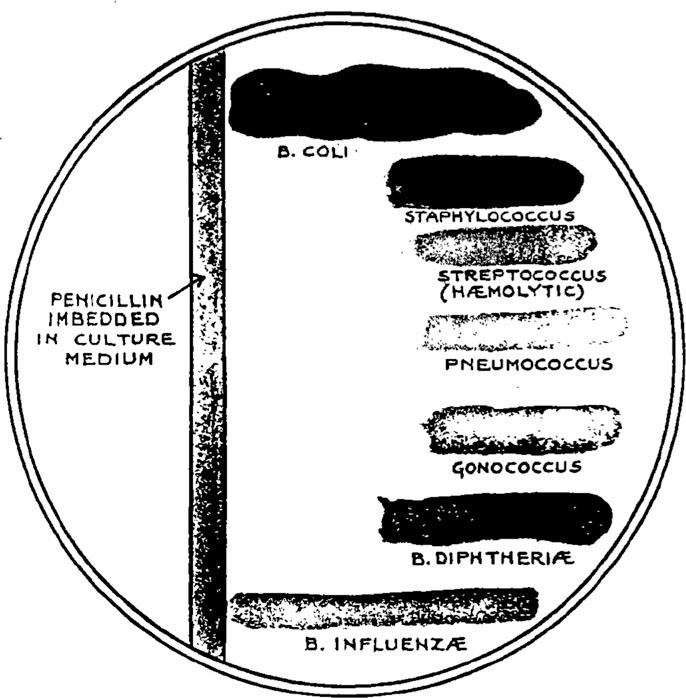
The discovery that penicillin was effective mostly against Gram-positive bacteria led researchers in the 1940s to look for other antibiotics that could kill Gram-negative bacteria. The first such broad-spectrum antibiotic was streptomycin, discovered in 1943 by Albert Schatz and Selman Waksman at Rutgers University. In addition to killing Gram-negative bacteria, streptomycin was the first effective treatment for the deadly bacterial disease tuberculosis. The reason for its effectiveness? Streptomycin has a chemical structure that allows it to pass more easily through the outer lipid layer of the Gram-negative bacterial cell wall. (Although natural penicillin cannot pass this layer, many modern synthetic varieties of penicillin, known collectively as beta-lactams, can.)
52
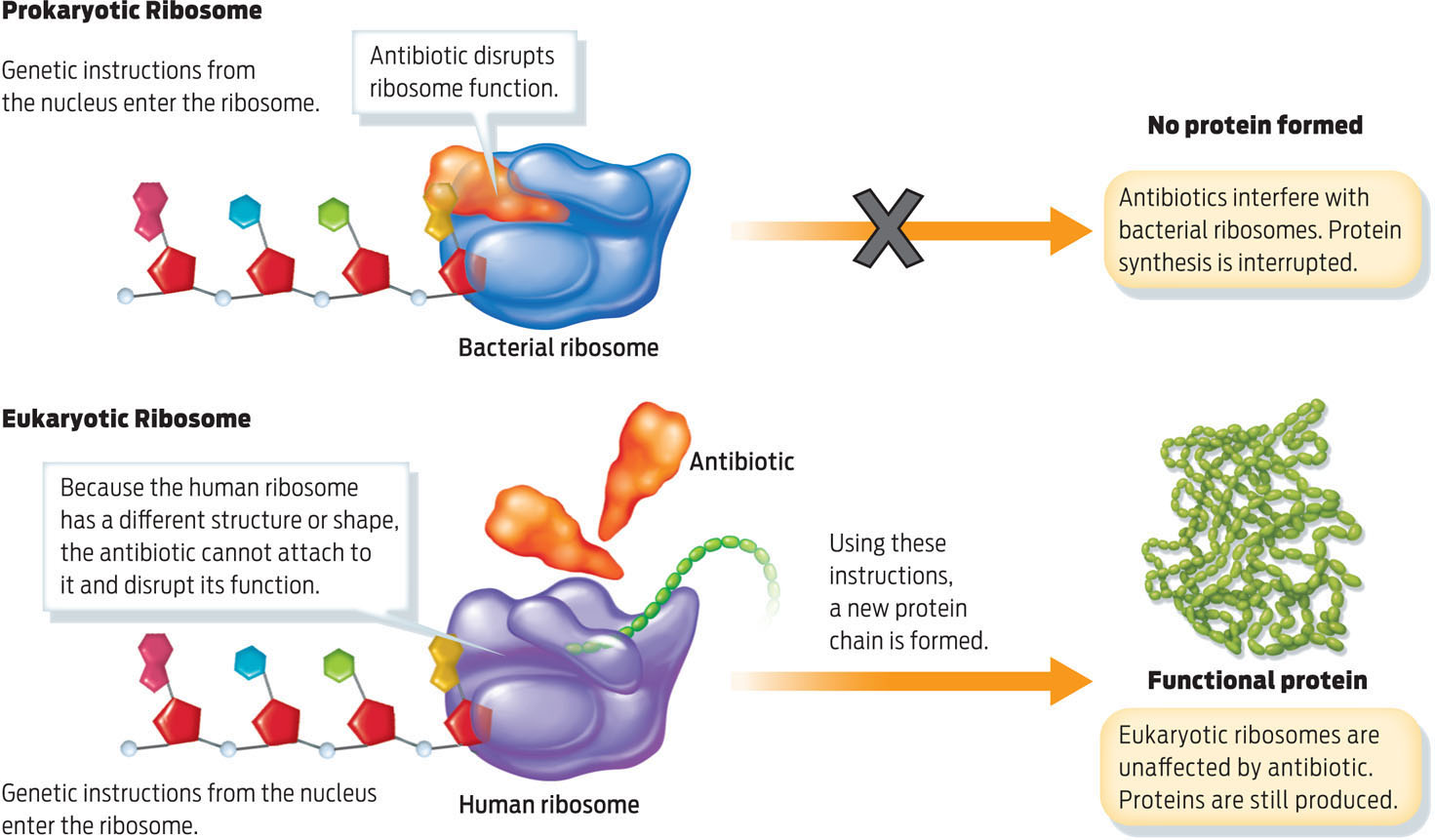
Once inside the cell, streptomycin works by interfering with protein synthesis on bacterial ribosomes. Ribosomes are the molecular “machines” that assemble a cell’s proteins. While both eukaryotic and prokaryotic cells have ribosomes, their ribosomes are of different sizes and have different structures. Because streptomycin targets features specific to bacterial ribosomes, it doesn’t harm the human who is taking it (INFOGRAPHIC 3.5).
Ribosomes are responsible for the synthesis of proteins in both prokaryotic and eukaryotic cells, but their structure is slightly different in the two types of cell. Antibiotics that interfere with prokaryotic ribosomes leave eukaryotic ribosomes unaffected.
Other antibiotics work in different ways-by inhibiting a bacterium’s ability to make a critical vitamin or to copy its DNA before dividing, for example. When this happens, the bacterium dies instead of reproducing.
53