3.6 Endocrine disruptors cause big problems at small doses.
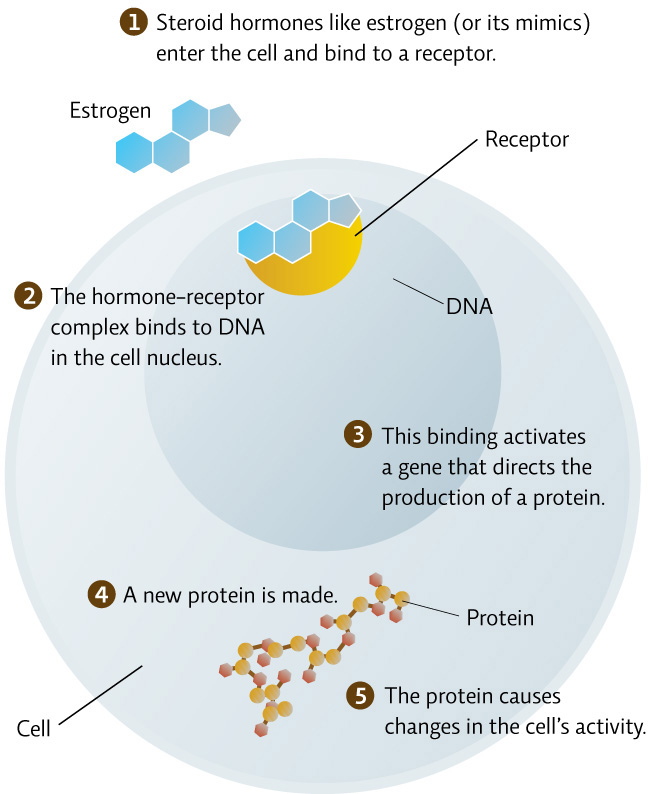
As their name suggests, endocrine disruptors interfere with the endocrine system, typically by mimicking a hormone, or preventing a hormone from having an effect. BPA is a mimic of estrogen, a hormone that plays many roles in the body, primarily guiding reproduction and development in both males and females. BPA binds to the body’s cellular estrogen receptors, among others, and triggers effects that natural estrogen would trigger. In animals living in the wild, chemicals like this have been shown to cause feminization of males (even sex changes), as evidenced by lower sperm counts and the production of egg proteins normally only produced by females.
In humans, we know that sperm counts are down among men and that puberty onset is earlier in both boys and girls than it has ever been before. We also know that 91% of the Canadian population has trace amounts of BPA in its urine. No one can say for sure whether one fact (changes in sexual development) is related to the other (BPA in our systems), but because hormones control the development of body organs, scientists are especially concerned about the exposure of developing fetuses, newborns, and infants to endocrine disruptors.
Endocrine disruptors are curiously different from many other chemicals, where the relationship between dose and effect is linear (the more you ingest, the sicker you get—“the dose makes the poison”). They can have one set of effects at a very low dose, and then no effects (or much different effects) at higher doses.
48
To track the effects of a dose of a chemical, toxicologists use data from in vitro and in vivo studies to create a dose-response curve, from which they can calculate an LD50 (lethal dose 50%), the dose that would kill 50% of the population. The lower the LD50, the more toxic the substance. [infographic 3.5]

Because endocrine disruptors like BPA have different effects at low and high doses, LD50s and dose-response curves are much trickier to calculate, and a “safe dose” is much tougher to determine. “We don’t know if BPA has a ‘threshold’ dose at which it starts to impact health,” says Bruce Lanphear, an epidemiologist and physician at Simon Fraser University, who studies the effects of BPA. Indeed, for endocrine disruptors, scientists have to test the effects of high doses and low doses separately.
In the late 1980s, when scientists were testing BPA, they started with very high doses, given to rats, lowered the dose until they saw no adverse effects, and then stopped. As is the usual practice, a “safe dose” was established by dividing that “no effect” level by 1000, to account for the possibility that humans might be more sensitive than lab animals, or that some people, such as children and the elderly or sick, might be more vulnerable than others.
But this strategy doesn’t necessarily apply to endocrine disruptors, where low doses can still cause harm. This was proven during one unfortunate chapter in our chemical history—between 1938 and 1971, doctors used the estrogen mimic diethylstilbesterol (DES) to prevent premature labour in expectant mothers. Thirty years later, when a higher incidence of reproductive abnormalities started showing up in the population, epidemiologists traced it back to the DES given to pregnant mothers.
49
Researchers actually developed BPA at the same time as DES—not as an ingredient of plastic, but as another estrogen mimic. They ended up shelving BPA when DES appeared to better replicate the effects of estrogen, says Lanphear. Only later did chemists discover that it had great sealant properties, making it useful for an infinite variety of products, from food and beverage cans to dental sealants and football helmets. Given this history, it should be no surprise that BPA has some effects on the human body, says Lanphear. “When you start to use chemicals, the first thing to ask is: does it have biological activities? And of course, BPA did, because that’s what it was designed to do.” [infographic 3.6]
Over the years, scientists have developed a list of BPA’s effects in lab animals: increased early growth in both males and females, early onset of sexual maturation in females, decreased testosterone and increased prostate size in males, altered immune function, and increased mortality of embryos. Increasingly, more experts began to worry that, at low doses—such as those quantities that leach from plastic containers into food and drinks—BPA might be particularly dangerous for pregnant mothers, developing fetuses, and young children.
Other researchers thought that developing fetuses were safe from any potential effects. They reasoned that BPA would be broken down in the mother’s gut and excreted in her urine long before it had a chance to reach the womb. Even if the gut failed, they thought, BPA would never get past the placenta. A 2002 study of 37 pregnant women, however, found BPA in fetal blood and the placenta.
So where did the truth lie?