13.1 An Introduction to Treatment
515
VOICES It’s a beautiful evening on the Rosebud Indian Reservation in south-

South Dakota is home to many American Indian tribes, including the Sicangu Lakota Oyate, or Rosebud Sioux. The Rosebud Indian Reservation is a vast and beautiful land, but its residents struggle with severe poverty—
516
LEARNING OBJECTIVES After reading and studying this chapter, you should be able to:
LEARNING OBJECTIVES After reading and studying this chapter, you should be able to:
LO 1 Outline the history of the treatment of psychological disorders.
LO 2 Discuss how the main approaches to therapy differ and identify their common goal.
LO 3 Describe how psychoanalysis differs from psychodynamic therapy.
LO 4 Outline the principles and characteristics of humanistic therapy.
LO 5 Describe person-
LO 6 Outline the principles and characteristics of behavior therapy.
LO 7 Outline the principles and characteristics of cognitive therapy.
LO 8 Summarize the biomedical interventions and identify their common goal.
LO 9 Describe how culture interacts with the therapy process.
LO 10 Identify the benefits and challenges of group therapy.
LO 11 Evaluate the effectiveness of psychotherapy.
LO 12 Summarize the strengths and weaknesses of online psychotherapy.
CONNECTIONS
In Chapter 3, we described sensation as the detection of stimuli by sensory organs. Stimuli are transduced into neural signals and sent to various parts of the brain. With hallucinations, the first step is not occurring (no apparent physical stimuli), but the sensory experience exists nevertheless. The brain interprets internal information as coming from outside the body.
Upon meeting with Chepa and her family, Dr. Foster realizes that she is having hallucinations, sensory experiences she thinks are real, but are not evident to anyone else. Chepa is also experiencing delusions, which are strange or false beliefs. And because she is vulnerable to acting on these hallucinations and delusions, she poses a risk to herself, and possibly others. Chepa needs to go to the hospital, and it is Dr. Foster’s responsibility to make sure she gets there, even if it requires going to a judge and getting a court order. “I’m going to make an intervention,” Dr. Foster offers, “and I’m going to have to do it in a way that’s respectful to that person and to the culture, but still respectful to the body of literature and training that I come from as a psychologist.”
Chepa’s grandmother protests: “I don’t want her going to the hospital. I want to use Indian medicine.” Trying to remain as clear and neutral as possible, Dr. Foster explains that if the voice were that of a spirit, it would have responded to prayer, pipe ceremony, and other traditional approaches. “I believe you’re hearing voices,” he says to Chepa. “But that voice is not coming from your uncle. . . . I think it’s coming from your own mind.” He goes on to describe how the brain has a region that specializes in hearing, and areas that store memories of people and their voices. It is possible, he explains, that the brain is calling forth a voice from the past, making it seem like it is here at this moment.
Note: Quotations attributed to Dr. Dan Foster and Laura Lichti are personal communications.
Chepa may not agree with Dr. Foster, but she trusts him. He is, after all, a relative. In Lakota culture, relatives are not necessarily linked by blood. One can be adopted into a family or community through a formal ceremony known as hunka. At Rosebud, all of the therapists and medical providers are linked to the community through hunka—
An ambulance arrives and transports Chepa to the emergency room, where she finds Dr. Foster waiting. He is there to make a diagnosis and develop a treatment plan, but also to provide her with a sense of security, and to do so in the context of a nurturing relationship. “First of all my concern is safety, and secondly my concern is that you realize I am concerned about you,” Dr. Foster says. “We’re going to form a relationship, you and I,” he says. “Whatever it is that we’re facing, we are going to make it so that it comes out better than it is right now.”
CONNECTIONS
In Chapter 12, we reported that schizophrenia is a persistent and debilitating disorder that affects approximately 0.3% to 1% of the population. In this chapter, we will present some approaches to treating people with this diagnosis.
The blood and urine screens come back negative, indicating that the hallucinations and delusions are not resulting from a drug, such as PCP or methamphetamine, and doctors find no evidence of a medical condition that could be driving the symptoms. Dr. Foster’s observations and assessments point to a complex psychological disorder known as schizophrenia.
517
Because Chepa poses an imminent risk to herself, Dr. Foster and his colleagues arrange a transfer to a psychiatric hospital, where she may stay for several days. The medical staff will stabilize her with a drug to help reduce her symptoms, the first of many doses likely to be administered in years to come. When she returns to the reservation, Dr. Foster and his colleagues will offer her treatment, which will be designed with her specific needs in mind. 
Dr. Dan Foster is the lead clinical psychologist on the Rosebud Reservation. He frequently works with clients suffering from severe emotional trauma, but he maintains a positive outlook. “I feel like the crucible of poverty and pain also is the crucible for transformation,” says Dr. Foster, who is a respected member of the Lakota community he serves.
Who Gets Treatment?
CONNECTIONS
In Chapter 12, we noted that stressors can impact the course of some psychological disorders. Periods of mania, depression, and psychosis can be brought on by life changes and stressors. The diathesis–
Therapists working on the Rosebud Reservation tend to see clients in crises, often related to the conditions of extreme poverty that exist on Northern Plains Indian reservations. The average unemployment rate is nearly 80% (United States Senate, 2010, January 28), and affordable housing is scarce. It is not unusual to have 14 or 15 relatives packed into living quarters the size of a two-
As you may already know, the arrival of European colonists in 1492 marked the beginning of a long, drawn-
518

Residents of the Rosebud Reservation gather for a powwow. Participating in cultural ceremonies and prayer may help people deal with stressors that could otherwise impact psychological problems.
CONNECTIONS
We discussed the etiology of psychological disorders in Chapter 12. The medical model implies that disorders have biological causes. The biopsychosocial perspective suggests disorders result from an interaction of biological, psychological, and sociocultural factors.
As we learn more about Dr. Foster’s work on Rosebud Reservation, be mindful that therapists work with a broad spectrum of psychological issues. Dr. Foster tends to work with people in severe distress. Some of his clients do not seek therapy, but end up in his care only because friends and relatives intervene. Other therapists spend much of their time serving people who seek help with issues such as shyness, low self-
Psychologists use various models to explain abnormal behavior and psychological disorders. As our understanding of psychological disorders has changed over time, so have treatments. While reading the brief history that follows, try to identify connections between the perceived causes of disorders and treatments designed to resolve them.
A Primitive Past: The History of Treatment
LO 1 Outline the history of the treatment of psychological disorders.
Psychological disorders are as old as recorded history, and some of the early attempts to “cure” and “treat” them were inhumane and unproven. One theory suggests that during the Stone Age, people believed psychological disorders were caused by possession with demons and evil spirits. Our cave dweller ancestors may have practiced trephination, or drilling of holes in the skull, perhaps to create exit routes for evil spirits (Maher & Maher, 2003).

American schoolteacher Dorothea Dix led the nation’s “mental hygiene movement,” an effort to improve the treatment of people living in mental institutions. Her advocacy work began in the mid-
ASYLUMS OR PRISONS? A major shift came in the 16th century. Religious groups began creating asylums, special places to house and treat people with psychological disorders. However, these asylums were overcrowded and resembled prisons, with inmates chained in dungeonlike cells, starved, and subjected to sweltering heat and frigid cold. During the French Revolution (the late 1700s), Philippe Pinel, a French physician, began working in Paris asylums. Horrified by the conditions he observed, Pinel removed the inmates’ chains and insisted they be treated more humanely (Hergenhahn, 2005; Maher & Maher, 2003). The idea of using “moral treatment,” or respect and kindness instead of harsh methods, spread throughout Europe and America (Routh & Reisman, 2003).
During the mid-
CONNECTIONS
In Chapter 12, we noted that most mental health professionals in the United States use the DSM–
In the early 1900s, psychiatrists began to realize that mental health problems existed outside asylums, among ordinary people who were capable of functioning in society. Rather than drawing a line between the sane and insane, psychiatrists began to view mental health as a continuum. They started developing a system to classify psychological disorders based on symptoms and progression, and this effort ultimately led to the creation of the first Diagnostic and Statistical Manual of Mental Disorders in 1952 (DSM; American Psychiatric Association, 1952; Pierre, 2012).
519
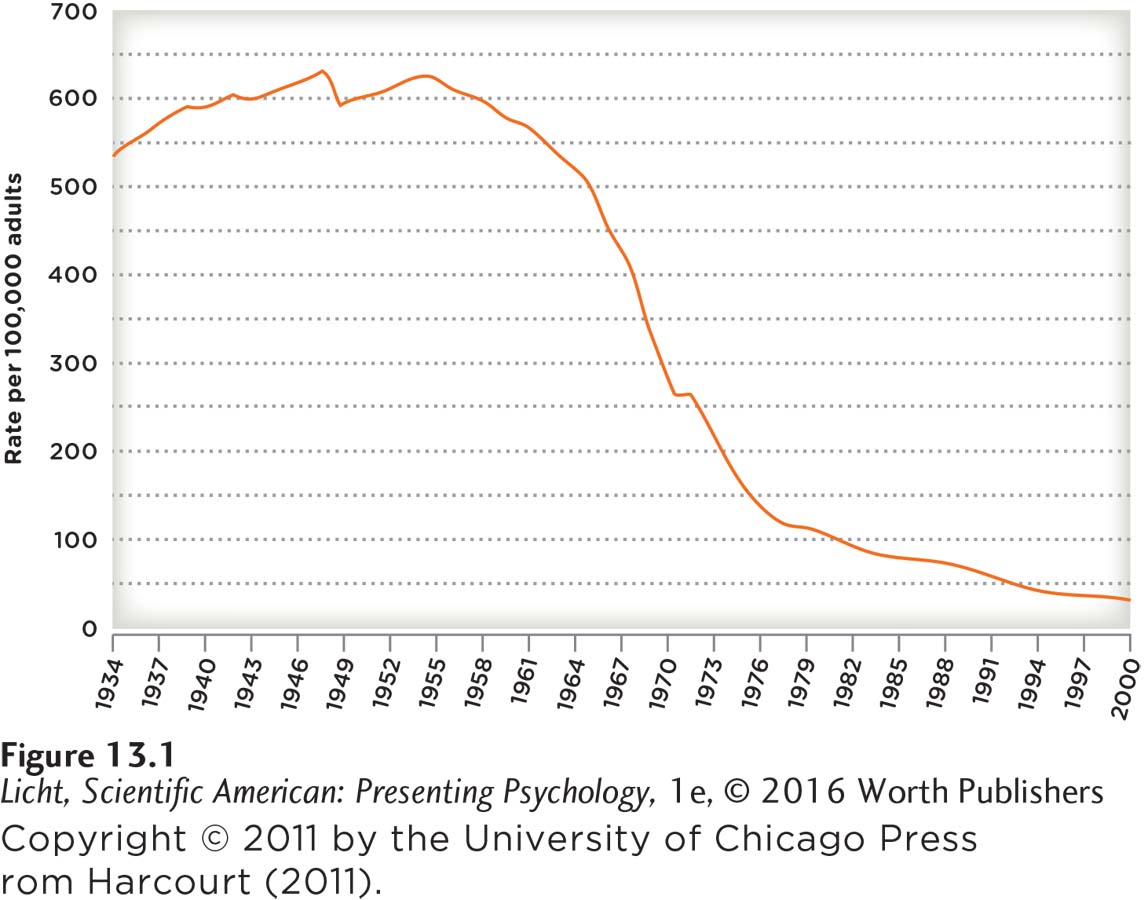
Since the 1950s, the rate of institutionalization has declined dramatically.
deinstitutionalization The mass movement of patients with psychological disorders out of mental institutions, and the attempt to reintegrate them into the community.
RETURN TO THE COMMUNITY The 1950s and 1960s in the United States saw a mass exodus of American patients out of institutions and back into the community (Figure 13.1). This deinstitutionalization was partly the result of a movement to reduce the social isolation of people with psychological disorders and integrate them into society. Deinstitutionalization was also made possible by the introduction of medications that reduced some symptoms of severe psychological disorders. Thanks to these new drugs, many people who had previously needed constant care and supervision began caring for themselves and managing their own medications—
CONNECTIONS
In Chapter 12, we described psychotic symptoms, such as hallucinations and delusions. Psychotic episodes can be risky for the person experiencing them—
In spite of the deinstitutionalization movement, psychiatric hospitals and institutions continue to play an important role in the treatment of psychological disorders. The scenario involving Dr. Foster and his client Chepa may be unusual in some respects, but not when it comes to the initiation of treatment. For someone experiencing a dangerous psychotic episode, the standard approach includes a stay in a psychiatric hospital or ward. Some of these admissions are voluntary; others are not.
Typically, a person is ready to leave the hospital after a few days or weeks, but many people in crisis are released after just a few hours, due to the high cost of treatment and financial pressures on hospitals. The length of a hospital stay is often determined by what insurance will cover, rather than what a patient needs, as well as the severe shortage of available beds in hospitals and units. Many psychiatric facilities simply cannot accommodate the scores of people seeking treatment (Honberg, Diehl, Kimball, Gruttadaro, & Fitzpatrick, 2011; Interlandi, 2012, June 22). We have come a long way in the treatment of psychological disorders, but there is still considerable progress to be made.
Treatment Today: An Overview of Major Approaches
520
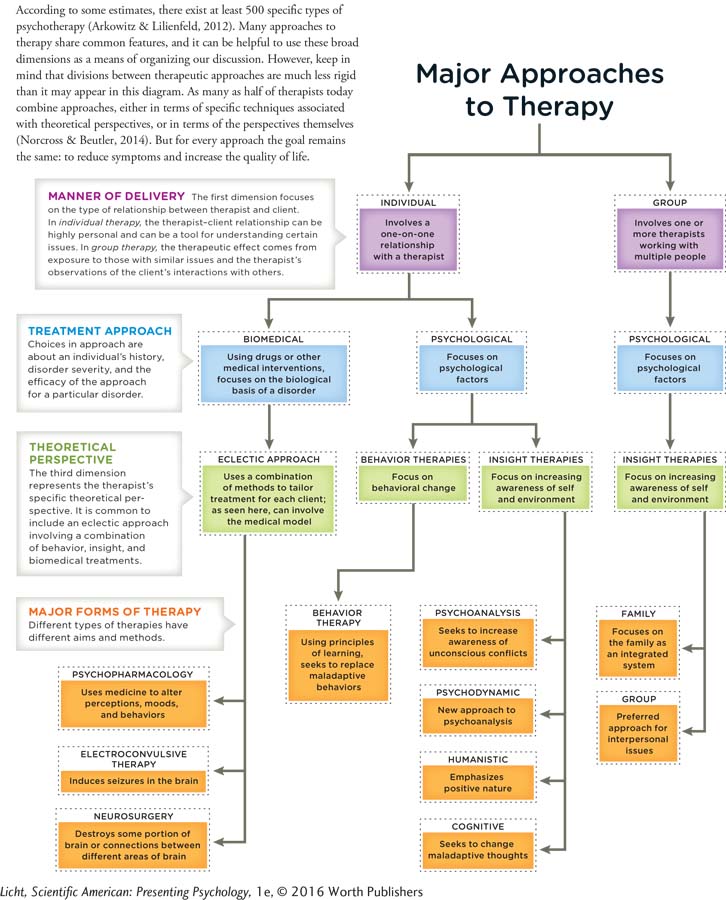
LO 2 Discuss how the main approaches to therapy differ and identify their common goal.
Today people receive treatment for a variety of reasons, not just mental disorders. Psychotherapy can help clients resolve work problems, cope with chronic illness, and adjust to major life changes like immigration and divorce. Some people enter psychotherapy to work on a specific issue or to improve their relationships.
The word psychotherapy derives from the Ancient Greek psychē, meaning “soul,” and therapeuō, meaning “to heal” (Brownell, 2010), and there are many ways to go about this healing of the soul. Some therapies promote increased awareness of situations and the self: You need to understand the origins of your problems in order to deal with them. Others focus on active steps toward behavioral change: The key to resolving issues is not so much understanding their origins, but changing the thoughts and behaviors that precede them. Finally, there are interventions aimed at correcting disorders from a physical standpoint. These treatments often take the form of medication, and may be combined with psychotherapy.
Many of these approaches share common features: The relationship between the client and the treatment provider is of utmost importance, as is a sense of hope that things will get better (Snyder et al., 2000). And they generally share a common goal, which is to reduce symptoms and increase the quality of life, whether a person is struggling with a psychological disorder or simply wants to be more fulfilled.
biomedical therapy Drugs and other physical interventions that target the biological processes underlying psychological disorders; primary goal is to reduce symptoms.
psychotherapy “Talk therapy”; a treatment approach in which a client works with a mental health professional to reduce psychological symptoms and improve quality of life.
insight therapies A type of psychotherapy, aimed at increasing awareness of self and the environment.
behavior therapies A type of therapy that focuses on behavioral change.
Synonyms
eclectic approach to therapy integrative approach to therapy
eclectic approach to therapy Drawing on multiple theories and approaches to therapy to tailor treatment for a client.
Psychological therapies can be categorized along three major dimensions (Infographic 13.1 on page 522). The first dimension is the manner of delivery—
522
INFOGRAPHIC 13.1
CONNECTIONS
In Chapter 1, we described the importance of operational definitions. An operational definition is the precise manner in which we define and measure a characteristic of interest. Here, it is important to create an operational definition of success, which allows for the comparison of different treatment approaches.
In addition to describing the various approaches to psychological treatment, we will examine how well they work. Outcome research, which evaluates the success of therapies, is a complicated task. First, it is not always easy to pinpoint the meaning of success, or operationalize it. Should we measure self-
show what you know
Question 1
1. Philippe Pinel was horrified by the conditions in Parisian asylums in the late 1700s. He insisted that the inmates’ chains be removed and that they be treated with respect and kindness. This _________________ then spread throughout Europe and America.
moral treatment
Question 2
2. A therapist writes a letter to the editor of a local newspaper in support of more funding for mental health facilities, stating that regardless of therapists’ training, all therapy shares the same goal of reducing _________________ and increasing the quality of life.
symptoms
combined approaches
biomedical therapy
the number of asylums
a. symptoms
Question 3
3. What were some of the consequences of deinstitutionalization?
Deinstitutionalization was the mass movement of patients with psychological disorders out of mental institutions, in an attempt to reintegrate them into the community. Deinstitutionalization was partially the result of a movement to reduce the social isolation of people with psychological disorders. This movement marked the beginning of new treatment modalities that allowed individuals to better care for themselves and function in society. However, many former patients ended up living on the streets or behind bars. Many people locked up in American jails and prisons are suffering from mental health problems.