9.2 Stimulants
Stimulants are named for their effect on the central nervous system: They stimulate it, causing increased activity and arousal. Stimulants include nicotine and amphetamines (including Ritalin), which are restricted, as well as cocaine, crack, and MDMA (Ecstasy, or “e”), which are illegal. At low doses, a stimulant can make the user feel alert, less hungry, and more energetic, mentally and physically.
In 1960, when the Beatles first started playing in Germany, they got through their performances by taking a legal stimulant, Preludin. A bouncer at the club simply handed pills to the boys and suggested that they take them. The pills had their effect: The musicians played for hours and then stayed up for hours afterward, going to other clubs (Spitz, 2005). And Preludin wasn’t the only stimulant that they took; they also drank coffee and tea and smoked cigarettes, all of which are legal stimulants.
What Are Stimulants?
In this section we first consider the illegal drugs cocaine and crack, and then we consider drugs that have both legal and illegal uses—amphetamines, methamphetamines, Ritalin, and MDMA.
Cocaine and Crack
Derived from the coca leaf, cocaine was a popular medicine for various ailments in 18th-century Europe and North America. Its use was declared illegal at the beginning of the 20th century, after it became clear that the drug was being abused and leading to tolerance and withdrawal (Rebec, 2000). Cocaine that is obtained in the form of a powder is typically inhaled, or “snorted”; as crack, a crystalline form, it is smoked.
Cocaine acts as a local anesthetic. Thus, when snorted, it leaves the user’s nose feeling numb; repeated snorting can lead to diminished sense of smell and difficulty swallowing (NIDA, 2007b). Although the first few experiences of cocaine use may provide a heightened sense of well-being that can last for up to an hour, this positive state becomes increasingly harder to attain as tolerance develops (NIDA, 2007b).
Higher doses of cocaine bring many negative effects: paranoia, to the point of delusions; hallucinations, such as feeling insects crawling on the body when there are none; compulsive, repetitive behaviors such as teeth grinding; and increased heart rate and blood pressure, with the accompanying risk of heart attack and sudden death. (The hallucinations occur because cocaine causes sensory neurons to fire spontaneously.) Users also lose their appetite, so people who have cocaine use disorder may develop malnutrition. TABLE 9.3 lists these and additional effects of regular cocaine use. People with cocaine use disorder often also have alcohol use disorder (Brady et al., 1995; Carroll et al., 1993; Regier et al., 1990); when these two substances are used at the same time, the risk of sudden death increases (NIDA, 2007b).
| Long-term effects of cocaine | Medical consequences of cocaine abuse |
|---|---|
|
Cardiovascular effects:
|
| Source: NIDA, 2004, p. 5. | |
Smoked crack acts more quickly than snorted cocaine and has more intense effects. Like snorting cocaine, smoking crack leads to a sense of well-being, energy, and mental clarity. However, this “high” usually lasts only minutes (NIDA, 2007b). As with other stimulants, when the high from crack is over, it leaves in its wake a sense of depression and craving for more of the drug, as related by Mr. R. in Case 9.1. These aftereffects may lead the user to take more of the drug and may lead to tolerance or withdrawal. Moreover, whereas tolerance of or withdrawal from cocaine may take months or even years of use to develop, such symptoms can develop extremely rapidly when people take crack—within weeks (NIDA, 2004; Rebec, 2000).
CASE 9.1 • FROM THE INSIDE: Cocaine Use Disorder—Crack
Mr. R, a 28-year-old man, describes his abuse of crack:
I first started using cocaine about 4 years ago. I don’t remember the first time I smoked the crack cocaine. It puts you in another world. I can’t explain this euphoric feeling that it gives you, but it’s a feeling I had never experienced before. I just want to sit there and enjoy the feeling and not think about anything or do anything. I have to keep doing it constantly to keep up the high.
I actually started staying out all night. I was smoking about five times a week and lost my apartment, lost everything. Everything was falling apart with my relationship, and I was starting to miss work a lot. But I just couldn’t control it. You know, it overtook me. That’s all I thought about and all I wanted to do was to keep smoking. Everything else was secondary.
An intense craving for me is when my heart starts beating fast—actually, I get a little sweaty—and all I think about doing is just going to smoke. That’s it. Nothing else—everything that’s on my mind just kind of disappears.
(Hyman, 2001, pp. 25–87)
As often happens when people develop a substance use disorder, Mr. R.’s life became focused on obtaining and using crack, and his intense cravings made it difficult for him to stop using the drug.
Amphetamines
Amphetamines typically produce the same effects as does cocaine, although these effects last longer. Common amphetamines include Benzedrine, Dexedrine, and Adderall. Amphetamines are usually available as pills, which typically are swallowed, although the contents of the pills may be snorted or diluted and injected. Amphetamines are legally used to treat some disorders, particularly ADHD and the sleep disorder narcolepsy, in which the sufferer spontaneously falls asleep for brief periods of time.
With repeated use of amphetamines, people may become hostile toward others, develop a sense of grandiosity, or exhibit disorganized thinking or behavior (Krystal et al., 2005). Because tolerance develops, repeat users may take high doses, which can cause amphetamine psychosis, a condition characterized by paranoid delusions and hallucinations (symptoms similar to those of paranoid schizophrenia; see Chapter 12). An amphetamine use disorder can have irreversible effects—including problems with memory and physical coordination—that arise from enduring changes in neurons (Volkow et al., 2001a), as well as reversible effects of irritability and violent behavior (Leccese, 1991; Wright & Klee, 2001). Withdrawal symptoms may include depression, fatigue, anxiety, and irritability.
Methamphetamine
Methamphetamine (“meth” or “speed”) is chemically similar to amphetamines but has a greater and longer-lasting effect on the central nervous system. It can be inhaled, swallowed, smoked, or injected, in all cases leading to an intense “rush” of pleasure. Use rapidly becomes use disorder.
In addition to causing irritability, heart problems, hallucinations and paranoia at high doses (McKetin et al., 2013; NIDA, 2007e), methamphetamine use can adversely affect the functioning of the neurotransmitters dopamine and serotonin, which leads to motor problems, impaired memory, and emotional dysregulation. Moreover, the increased blood pressure that results from taking the drug can cause strokes (NIDA, 2007e; Thompson et al., 2004). TABLE 9.4 summarizes the effects of long-term methamphetamine abuse. Some—but not all—of the brain damage inflicted by methamphetamine abuse is reversible with long-term abstinence (Salo et al., 2011; Volkow et al., 2001a).
|
| Source: Adapted from NIDA, 2008c. |
Ritalin
Ritalin (methylphenidate hydrochloride) is frequently prescribed for ADHD. Its neurological effect is similar to, but slower than, that of cocaine. People who abuse Ritalin take the stimulant in any of three ways:
- swallowing pills, which does not usually lead to use disorder;
- inhaling or snorting crushed pills, which leads to a quicker “high” and causes lung problems; or
- injecting the drug in liquid form, which produces an effect similar to that of cocaine.
Both inhaling and injecting Ritalin can lead to use disorder. People who do not have ADHD may occasionally swallow Ritalin pills for the stimulant effects—heightened alertness, increased attention, and decreased appetite. Although such casual use does not meet the criteria for a use disorder, it still carries the risk of adverse medical side effects, including heart problems and stroke.
MDMA (Ecstasy)
Methylenedioxymethamphetamine (MDMA), commonly called Ecstasy or simply “e,” is usually taken in tablet form. It is chemically similar both to methamphetamine and to the hallucinogen mescaline, and it has the effects of both types of drugs: the stimulant effect of increased energy and the hallucinogenic effect of distorted perceptions. When first using it, people report heightened feelings of well-being, empathy, and warmth toward others, and a greater sensitivity to touch. This experience is less pervasive with subsequent use. Other effects are reduced anxiety and distorted time perception (NIDA, 2007e). Abuse can result in poor mood and difficulty regulating emotions, as well as anxiety and aggression, sleep problems, and decreased appetite (NIDA, 2008b).
In addition, MDMA users can develop impaired cognitive functioning, especially problems with memory, after the drug wears off. These cognitive deficits become more severe when the drug is abused (Verkes et al., 2001). One survey of MDMA users found that almost 60% reported withdrawal symptoms that included poor concentration, depression, decreased appetite, and fatigue; moreover, almost half of these users developed MDMA use disorder (NIDA, 2007e; Stone et al., 2006). Frequent users of MDMA may experience tolerance and withdrawal symptoms (Leung & Cottler, 2008). Lynn Smith, in Case 9.2, recounts her experience of MDMA use disorder.
CASE 9.2 • FROM THE INSIDE: MDMA Use Disorder
Sometimes I stopped eating and sleeping. I worked only two days a week to support my habit. The rest of the time was spent getting high, almost always on Ecstasy. The utter bliss of my first Ecstasy experience was a distant memory. Of course, I never could recapture that first high, no matter how much Ecstasy I took.
In five months, I went from living somewhat responsibly while pursuing my dream to a person who didn’t care about a thing—and the higher I got, the deeper I sank into a dark, lonely place. When I did sleep, I had nightmares and the shakes. I had pasty skin, a throbbing head and the beginnings of feeling paranoid. (Partnership for a Drug-Free America, 2007)
MDMA’s side effects are similar to those of other stimulants, including increased blood pressure and heart rate. Excessive sweating, another side effect, can cause acute dehydration and hyperthermia (abnormally high body temperature). The effects of MDMA may be difficult to predict in part because the tablets often contain other drugs, such as ketamine, cocaine, or other stimulants (Green, 2004).
“Bath Salts”

Another type of stimulant is commonly known as bath salts. These drugs are not to be confused with traditional bath salts, such as Epsom salts, which are used to enhance the experience of soaking in a bathtub; those bath salts are not psychoactive substances. Stimulant bath salts are a family of drugs that contains a chemical related to cathinone, which is found in the khat plant; it is chemically similar to amphetamines and Ecstasy. However, the exact composition of each packet of bath salts varies, and packets typically contain at least one other type of drug, such as MDMA. Bath salts may lead some users to feel more outgoing and happy, but other users become agitated and paranoid and even hallucinate or become violent (Penders et al., 2012). Users—even those who have had an unpleasant experience—report intense cravings for more of the substance (Slomski, 2012). Bath salts are typically sold as a powder, which is swallowed, inhaled, or injected; adverse effects occur most often when bath salts are snorted or injected (NIDA, 2012).
Bath salts increase the activation of dopamine and may kill neurons (Slomski, 2012). Users of bath salts may need to go to a hospital emergency room because of medical symptoms such as chest pains or racing heart or because of psychological symptoms such as hallucinations, paranoia, or panic attacks. Some people have died as a result of the side effects of using bath salts.
Understanding Stimulants
For the most part, use disorders of the different stimulants arise for similar reasons; thus, in what follows we will consider the roles of the three kinds of factors in leading to use disorders of all stimulants.
Brain Systems and Neural Communication: Dopamine and Abuse
Dopamine plays a key role in both the pleasurable experience of taking stimulants and the abuse of stimulants (Kalivas & Volkow, 2005). To see how, we need to consider the neural circuits that rely on dopamine. To begin, let’s consider one classic study. Researchers placed tiny electrodes in parts of rats’ brains; when the rats pressed a lever, they got a small jolt of electricity, which activated neurons near the electrodes (Olds & Milner, 1954). The researchers discovered that the animals worked hard to receive electrical stimulation to certain parts of the brain. In fact, they sometimes seemed to prefer such stimulation to food or drink! (This cannot help but remind us of some forms of drug abuse, in which users sacrifice food and drink for the drug.) This sort of finding eventually led researchers to define a “reward system” in the brain. This reward system includes the ventral tegmental area, which in turn activates the nucleus accumbens (see Figure 9.3). The neurons in this system rely on the neurotransmitter dopamine. In fact, if animals are given a drug that blocks the effects of dopamine, they will not work as hard to receive electrical stimulation in these areas (Fibiger & Phillips, 1988). For this reason, the reward system is usually referred to as the dopamine reward system. A wide range of pleasurable activities, such as eating and having sex, activate the dopamine reward system.
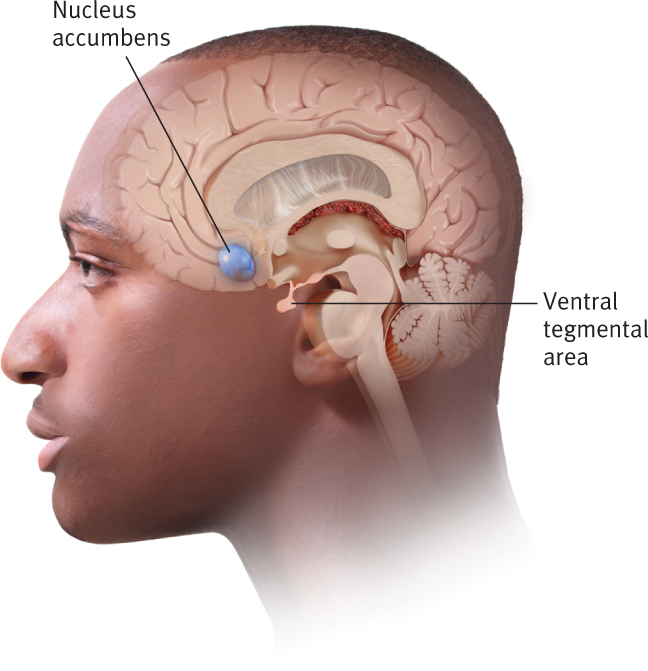
Dopamine reward system The system of neurons, primarily in the nucleus accumbens and ventral tegmental area, that relies on dopamine and gives rise to pleasant feelings.
All stimulant drugs affect the dopamine reward system directly (Tomkins & Sellers, 2001). Many other substances (e.g., alcohol) also activate the dopamine system directly, and still other types of substances activate it indirectly by altering other brain areas or neurotransmitters that, in turn, affect dopamine (Leone et al., 1991). Researchers have thus proposed the dopaminergic hypothesis of substance abuse: The rewarding effects of a drug arise from the dopamine reward system (Koob & Le Moal, 2008; Robbins & Everitt, 1999a, 1999b; Tomkins & Sellers, 2001).
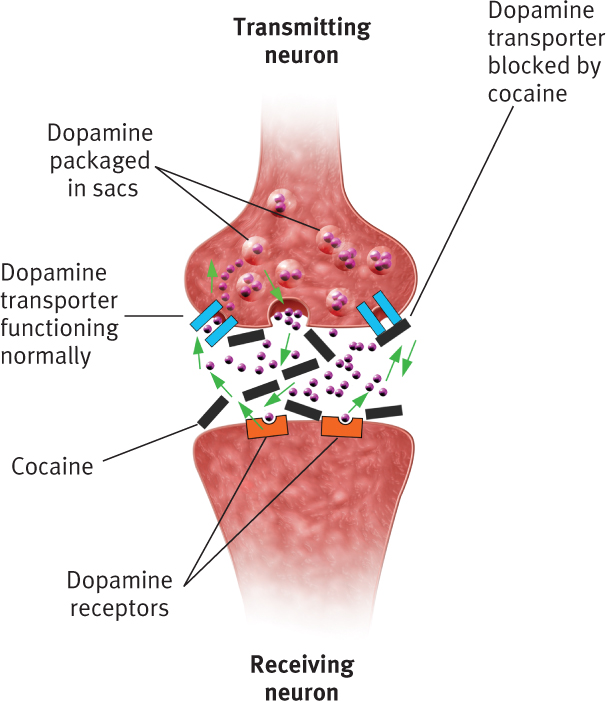
Because of the neural changes that occur with continued abuse, after a while, the person needs the substance to feel “normal” and experiences cravings when not using the drug. Moreover, larger doses of the drug are necessary to experience pleasure. For example, consider how cocaine affects neurons in the dopamine reward system: Cocaine binds to dopamine transporters—the molecules that take excess dopamine from the synapse and bring it back to dopamine-containing sacs within the terminal buttons of the transmitting neuron (see Figure 9.4). When cocaine binds to these transporter molecules, the transporters don’t operate as effectively to remove dopamine from the synapses—and thus more dopamine lingers there, which causes the receptors on the receiving neuron to become less sensitive. Thus, larger doses of the drug are needed to produce more dopamine before it produces pleasurable sensations.
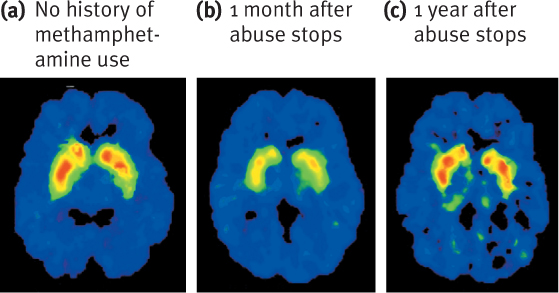
A similar mechanism is at work when someone takes methamphetamine. Again, the drug binds to the molecules that transport excess dopamine back to the terminal buttons and prevents reuptake from operating effectively—thereby leaving more dopamine in the synapse, which in turn leads the dopamine receptors eventually to become desensitized. Moreover, as shown in Figure 9.5, not all of the damage inflicted on the brain by long-term methamphetamine use is reversible. The images in the figure show the distribution of dopamine transporters in the brain of a person who abused methamphetamine. As is evident, even 2 years after the person stopped using methamphetamine, the neurological effects of chronic abuse are not totally reversed.
As researchers have come to understand the dopamine reward system in more detail, they have begun to gain insight into an age-old puzzle: Are some people more susceptible to developing a use disorder because they have less “character” or a weak “moral compass”? No. In fact, at least part of the answer is that the dopamine reward system is more sensitive and responsive in some people. For example, in one study, participants were given an injection of the stimulant Ritalin; participants who rated the experience as pleasant had fewer dopamine receptors in their brains than those who found it unpleasant (Volkow et al., 1999). Such findings support the hypothesis that people with fewer dopamine receptors may be more vulnerable to drug use (and use disorders); the smaller quantity of receptors means they have reduced activation in the reward system, which is boosted by substance use (Swanson & Volkow, 2002).
However, we want to end this section with an observation: As we’ve noted previously, brain areas work together in systems and often more than one system is involved in producing a particular behavior. This is true of use disorders of stimulants in particular and substance use disorders in general. Although the dopamine reward system plays a crucial role in leading people to abuse drugs, many other neurotransmitters and their related brain systems have been implicated in drug abuse, particularly gamma-aminobutyric acid (GABA), glutamate, and serotonin. TABLE 9.5 lists the neurological factors that contribute to use disorders of stimulants.
|
| *This factor is not unique to stimulant use disorders. |
Psychological Factors: From Learning to Coping
Various psychological factors contribute to use disorders of stimulants and to substance use disorders in general. In what follows we examine these psychological factors in more detail.
Operant Conditioning
Reward craving The desire for the gratifying effects of using a substance.
Operant conditioning influences stimulant use and whether a person will develop a substance use disorder in several ways. First, if stimulant use is followed by pleasant consequences, those consequences act as positive reinforcement (which leads to recurrent use). Research on the dopamine reward system shows that aspects of this type of learning have neurological underpinnings. In fact, the dopamine reward system begins to be activated with the expectation of a drug’s positive effects (that is, the expectation of reinforcement), which leads to a specific type of craving, reward craving—the desire for the gratifying effects of using a substance (Verheul et al., 1999).
Second, using stimulants can independently lead to negative reinforcement—alleviating a negative state, thereby producing a desirable experience. (Remember that negative reinforcement is not the same as punishment.) In fact, such negatively reinforcing effects contribute to substance use disorders among people trying to manage the psychological aftereffects of physical or emotional abuse (Bean, 1992; Catanzaro & Laurent, 2004; Ireland & Widom, 1994); in particular, using drugs may (temporarily) distract them from painful memories or their present circumstances and hence be reinforcing.
Relief craving The desire for the temporary emotional relief that can arise from using a substance.
The temporary emotional relief provided by substance use can create cravings for the drug when a person experiences negative emotions; this type of craving is sometimes referred to as relief craving (Verheul et al., 1999). Both reward craving and relief craving can cause people to use drugs compulsively, even when they would like to quit. Thus, cravings of both types are thought to play a primary role in maintaining substance use disorders, and having such cravings is one of the criteria for this category of disorders (American Psychiatric Association, 2013; Torrens & Martín-Santos, 2000).
A third way that operant conditioning contributes to substance use disorders also involves negative reinforcement, but in this case it occurs because using the substance can eliminate withdrawal symptoms, which can range from mildly unpleasant to extremely unpleasant and potentially lethal. Substance use eliminates the unpleasant withdrawal state, which increases the likelihood of subsequent use.
Classical Conditioning
Drug cues The stimuli associated with drug use that come to elicit conditioned responses through their repeated pairings with use of the drug.
Stimuli associated with drug use (such as drug paraphernalia or the music and crowds at a club) are referred to as drug cues, and they come to elicit conditioned responses through their repeated pairings with drug use. Connections among different brain areas, such as the amygdala and hippocampus, store such associations between drug use and the stimuli related to drug use. The drug cues are then associated with the reinforcing (positive or negative) effects of the drug; once such associations are established, these drug-related stimuli themselves can trigger the dopamine reward system (Tomkins & Sellers, 2001). That is, classical and operant conditioning interact: When the consequences (effects) of drug use are rewarding, the person is likely to use drugs again and again. Repeated drug use, in turn, can produce classical conditioning, whereby stimuli associated with drug use, such as the vial containing crack, elicit a craving for the drug (Epstein et al., 2009). Such factors affect each other and can become feedback loops that create a spiral of a substance use disorder. For example, people often handle money when buying cocaine and then use the cocaine shortly afterward; handling money can then become a conditioned stimulus. Thus, a person addicted to cocaine can come to crave it after handling money (Hamilton et al., 1998).
Moreover, simply imagining drug cues can activate structures in the limbic system (Dackis & O’Brien, 2001), which is tightly tied to the dopamine reward system, and lead to drug cravings (Hyman, 2005; Stewart et al., 1984). Even after successful treatment for substance use disorders, being exposed to drug cues can lead a former abuser to experience powerful cravings and can increase the risk of relapse (Hyman, 2005; Torrens & Martín-Santos, 2000). Cravings do not last indefinitely, however. When a person craves a substance but does not use it, the craving normally disappears within an hour (Wertz & Sayette, 2001). Researchers have found that a person is more likely to feel the craving when he or she expects to be able to take the drug.
TABLE 9.6 summarizes the psychological factors that contribute to use disorders of stimulants.
|
| *This factor is not unique to stimulant use disorders. |
Social Factors
Various social factors can promote substance use disorders, such as patterns of family interactions and perceived social norms. Moreover, sociocultural factors increase the vulnerability of some people for developing use disorders of stimulants and substance use disorders in general.
Family Relations and Peers
Research grounded in the stage theory (introduced earlier in this chapter) found that teenagers whose drug use progressed from marijuana to other illegal substances did not have close relationships with their parents (Andrews et al., 1991). However, this finding is only a correlation; it could be that the factors that led to a use disorder also soured relationships between teenager and parents or that bad relationships contributed to drug abuse—or that some third factor, such as a particular temperament, contributed to both factors. In addition, many studies have found that adolescents who have dysfunctional family interactions (for example, have experienced child abuse, violence in the household, or parental substance abuse) are more likely to use and abuse substances (Becoña et al., 2012; Hawkins et al., 1992; Kilpatrick et al., 2000).
A person’s family members can affect whether he or she comes to use or abuse substances. For instance, when older siblings use drugs, their closer-in-age younger siblings are more likely to do the same than are their further-apart-in-age younger siblings. And within the first year of when a spouse registers with a drug problem, his or her partner is at increased risk of abusing drugs (Kendler, Ohlsson, et al., 2013).
Another social factor involves peers. Friends do things together; they often have common views or activities they enjoy. It’s not surprising, then, that peers’ substance use can influence a friend’s use and abuse of psychotropic substances (Brewer et al., 1998; Keyes et al., 2012). Studies have found that if a person’s peers use or abuse substances, that person is likely to do the same (Dishion & Medici Skaggs, 2000; Fergusson et al., 2002). The influence of peers can also help explain findings that support the gateway hypothesis about increasing drug use. Once a (susceptible) person repeatedly uses an illicit entry drug, such as marijuana, he or she is then more likely to spend time with peers who also use this drug and become socialized into a subculture favorable to drug use.
Norms and Perceived Norms
Societies specify norms of behavior, which include the degree to which psychoactive substances can be taken without being considered a use disorder. The Beatles changed the social norms, at least for a while, of some portions of the population through their public association with drugs: Their arrests for possession of illegal drugs, Paul McCartney’s admission that he used LSD, and song lyrics referring to drug use (such as, “I get high with a little help from my friends”). Many fans perceived that drug use was “in” and that they would not be “cool” unless they used drugs, too.
This observation highlights an important fact about social norms: It’s a person’s perception of the norms, not the actual social norms, that is the key. That is, when people think that “everyone” in their school, neighborhood, social class, or clique uses drugs, they are more likely to use drugs themselves. In contrast, people who think that only a minority of their classmates, neighbors, or friends use drugs will be less likely to use drugs. In fact, just watching movies can be enough to shift perceptions of social norms. For example, teenagers who watch movies in which the characters drink are more likely to binge drink themselves (Hanewinkel et al., 2012). The extent of the group’s actual drug use is less important than what the person perceives it to be.
GETTING THE PICTURE

Jenkedco/Shutterstock
Sociocultural Factors
In addition to family and friends, other social forces can nudge individuals closer to or further away from a stimulant use disorder as well as substance use disorders in general. People who are experiencing economic hardship and are unemployed are at increased risk of developing substance use disorders (Reid et al., 2001; SAMHSA, 2000). Consider that children who grow up in economically disadvantaged neighborhoods are more likely to be exposed to ads for legal psychoactive substances (alcohol and cigarettes) and to have easier access to these legal psychoactive substances as well as to illegal ones. Children who live in such neighborhoods may also observe more abuse of substances among family members, peers, or adults; as noted earlier, such modeling can have an adverse effect. Moreover, these children are also more likely to experience or witness traumatic events and develop PTSD (see Chapter 7), which is associated with substance use disorders (Johnson, 2008; Stewart, 1996).
Society at large also influences substance use by establishing legal consequences (Torrens & Martín-Santos, 2000). Society’s influence is also seen in how access to drug treatment centers is regulated and in the national policies that direct resources toward effective prevention and treatment programs. TABLE 9.7 summarizes the social factors associated with stimulant use disorder.
|
| *This factor is not unique to stimulant use disorders. |
As noted by the asterisks in Tables 9.5, 9.6, and 9.7, most of the factors that contribute to use disorders of stimulants also contribute to use disorders of other substances; the one exception is the specific neurological effects of stimulant drugs. Because most of the factors contribute to substance use disorders generally, we do not examine the feedback loops among the factors until after we review all types of substance use disorders.
Thinking Like A Clinician
One night before a major class project was due, Sierra had hours of work left to do, and she’d had all the coffee she could stand. She took one of her roommate’s Ritalin pills and stayed up all night, completing the project by morning. Sierra gradually got in the habit of using amphetamines to help her stay up late and do course work. After college, Sierra took a job with lots of deadlines and lots of late hours. She continued to use stimulants to help her work, sometimes taking cocaine when she could get it.
At what point would Sierra’s use of stimulants become a use disorder? What would be some specific symptoms that would indicate that she had cocaine use disorder? What symptoms would you expect to see if Sierra were taking a high dose of stimulants? According to the neuropsychosocial approach, what factors might have led Sierra to abuse stimulants, if she were abusing them?