
 DRIVING QUESTIONS
DRIVING QUESTIONS
- What is staph, and can it be present in the absence of an infection?
- How do bacteria resist the effects of antibiotics?
- How do populations evolve, and what is the role of evolution in antibiotic resistance?
In-Class Activity
Click here to access Lecture ppt specifically designed for chapter 14.
Click here to access Clicker Questions specifically designed for chapter 14.
 N JANUARY 2008, SIXTH-GRADER CARLOS DON, AN ACTIVE footballer and skateboarder, boarded a bus headed for a class trip, happy and healthy. A month later he was dead.
N JANUARY 2008, SIXTH-GRADER CARLOS DON, AN ACTIVE footballer and skateboarder, boarded a bus headed for a class trip, happy and healthy. A month later he was dead.
In April 2006, 17-year-old Rebecca Lohsen was a model student at her high school; she was on the honor roll and was a member of the swim team. Four months later Rebecca was dead.
In December 2003, Ricky Lannetti was a college senior, a star football player and all-around athlete. A few weeks later Ricky was dead.
Scientists are now seeing bacterial infections that don’t respond to any known antibiotics, leading many to fear the day when we run out of treatment options altogether.
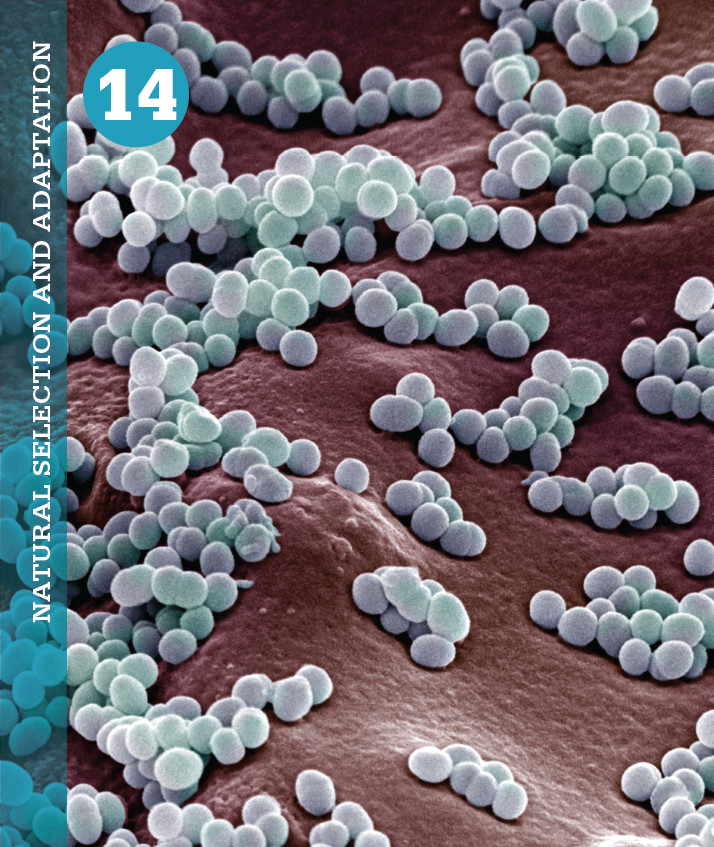
The list of sudden deaths like these goes on and on. But surprisingly, these young people weren’t killed in accidents or by violence; they were all killed by an infectious bacterium known as methicillin-resistant Staphylococcus aureus (MRSA), which has become widespread in recent years and which is difficult to treat with many existing antibiotics.
MRSA (pronounced “mer-sa”) sickens some 94,000 people in the United States each year and kills almost 19,000, according to a 2007 study by Monina Klevens and her colleagues at the Centers for Disease Control and Prevention (CDC). Formerly, outbreaks of MRSA were confined mainly to hospitals. But since the late 1990s, a growing number of healthy people are becoming infected outside hospitals. In addition, new high-risk groups are emerging—children in day care, the prison population, men who have sex with men, and certain ethnic groups—whose MRSA infection rates are higher than those in the general population. Schools nationwide have been reporting outbreaks and young, healthy people are getting sick.
For more than 60 years, bacteria-caused infections have been successfully combated with antibiotics—those “wonder drugs” that Alexander Fleming first discovered in a moldy petri plate nearly a century ago (see Chapter 3). But many of our most trusted antibiotics are no longer effective at killing the bacteria they once defeated. Over time, these bacteria have changed genetically—evolved—to become resistant. As a result, scientists are now seeing bacterial infections that don’t respond to any known antibiotics, leading many to fear the day when we run out of treatment options altogether.
“This is a major public health imperative,” says Robert Daum, professor of microbiology at the University of Chicago and a member of the Infectious Diseases Society of America. “We need a plan of attack now.”