CHAPTER 31 Test Your Knowledge
DRIVING QUESTION 1
What is the structure of a virus, and how do viruses cause disease?
By answering the questions below and studying Infographics 31.1 and 31.5, you should be able to generate an answer for the broader Driving Question above.
KNOW IT
 Which of the following is found in all viruses?
Which of the following is found in all viruses?
a. DNA
b. RNA
c. a membranous envelope
d. a protein shell
e. a cell membrane
d
 Explain how viruses replicate within humans.
Explain how viruses replicate within humans.
Viruses must enter their specific host cell in the human, thus infecting it. Once they have entered the host cell, they use host cell resources and direct the host cell to replicate the virus.
 Why does poliovirus cause long-lasting damage, whereas those infected by influenza virus typically make a full recovery?
Why does poliovirus cause long-lasting damage, whereas those infected by influenza virus typically make a full recovery?
Poliovirus infects and damages nerve cells. As nerve cells do not replicate, they cannot repair themselves. Influenza virus infects cells lining the respiratory tract, which are replaced at high frequency.
USE IT
 Both viruses and bacteria can be human pathogens. Describe some key differences between them. (Hint: You may wish to refer to Chapter 14.)
Both viruses and bacteria can be human pathogens. Describe some key differences between them. (Hint: You may wish to refer to Chapter 14.)
Viruses are not made of cells, and cannot replicate on their own. Instead, they must infect a host cell in order to replicate. Bacteria are prokaryotic organisms, and most are capable of replicating on their own.
 Why do poliovirus, influenza virus, and HIV infections cause different symptoms?
Why do poliovirus, influenza virus, and HIV infections cause different symptoms?
Each infects a different host cell. Poliovirus infects cells of the nervous system, causing paralysis. Influenza virus infects cells of the respiratory tract, causing respiratory tract symptoms. HIV infects cells of the immune system, causing an immune deficiency.
DRIVING QUESTION 2
What is innate immunity?
By answering the questions below and studying Infographics 31.3 and 31.4, you should be able to generate an answer for the broader Driving Question above.
KNOW IT
 Name three components of the innate immune system. For each, provide a brief description of how it offers protection.
Name three components of the innate immune system. For each, provide a brief description of how it offers protection.
Skin provides a barrier to pathogen entry; Enzymes in tears and saliva digest components of pathogens. Phagocytes ingest and destroy pathogens.
 What do macrophages and neutrophils have in common?
What do macrophages and neutrophils have in common?
They are both specialized white blood cells (macrophages are found in tissues, neutrophils circulate in the blood), and they are both phagocytes.
USE IT
 From what you know about innate immunity, would you predict different or identical innate responses to infections from E. coli (a bacterium) and S. aureus (another bacterium)? Explain your answer.
From what you know about innate immunity, would you predict different or identical innate responses to infections from E. coli (a bacterium) and S. aureus (another bacterium)? Explain your answer.
As innate immunity is nonspecific (it does not uniquely recognize different pathogens), the innate response to E. coli will be the same as the innate response to S. aureus.
 Neutropenia is a deficiency of neutrophils. Would you expect someone with neutropenia to be able to mount an effective inflammatory response? Explain your answer.
Neutropenia is a deficiency of neutrophils. Would you expect someone with neutropenia to be able to mount an effective inflammatory response? Explain your answer.
As neutrophils are important phagocytes in the inflammatory response, someone who is deficient in neutrophils will not be able to mount an effective inflammatory response.
 Why might someone taking anti-inflammatory drugs be more susceptible than others to bacterial infections?
Why might someone taking anti-inflammatory drugs be more susceptible than others to bacterial infections?
As the inflammatory response is important in killing and containing pathogens at their sites of entry, someone taking anti-inflammatory drugs will be more vulnerable to infections because an important component of their innate defenses will have been suppressed by the drugs.
DRIVING QUESTION 3
What is adaptive immunity, and how does vaccination rely on adaptive immunity?
By answering the questions below and studying Infographics 31.3, 31.6, 31.7, 31.8, and 31.9, you should be able to generate an answer for the broader Driving Question above.
KNOW IT
 Compare and contrast the features of innate and adaptive immunity.
Compare and contrast the features of innate and adaptive immunity.
Innate immunity is present since birth, always active and nonspecific. It does not have “memory.” Adaptive immunity is specific for a particular pathogen and must be turned on when the specific pathogen is encountered— it is not always “on”). Adaptive immunity exhibits “memory,” strengthening with repeated exposures to the same pathogen.
 B cells, plasma cells, and antibodies are all related. Describe this relationship, using words, a diagram, or both.
B cells, plasma cells, and antibodies are all related. Describe this relationship, using words, a diagram, or both.
B cells are lymphocytes that are activated during an adaptive response. Upon activation, they specialize into antibody-producing plasma cells. The antibodies produced then specifically bind to and inactivate their targets.
USE IT
 Anti-hepatitis C antibodies present in a patient’s blood indicate
Anti-hepatitis C antibodies present in a patient’s blood indicate
a. that the patient is mounting an innate response.
b. that the patient has been exposed to HIV.
c. that the patient has been exposed to hepatitis C within the last 24 hours.
d. that the patient has been exposed to hepatitis C at least 2 weeks ago.
e. that the patient has hepatitis.
d
 Vaccination against a particular pathogen stimulates what type of response?
Vaccination against a particular pathogen stimulates what type of response?
a. innate
b. primary
c. secondary
d. autoimmune
e. b and c
e
 Will someone who has been exposed to seasonal influenza in the past
Will someone who has been exposed to seasonal influenza in the past
a. have memory B cells?
b. still be at risk for seasonal influenza next year? Why?
c. still be at risk for H1N1 (swine flu)? Why?
a: Yes. They will have memory B cells specific for the influenza virus they were exposed to. b: Yes. They are still at risk for next year’s seasonal flu. The flu varies seasonally as a result of mutations, so their memory cells won’t recognize the strain of seasonal flu circulating next year. c: Yes. They are still at risk for H1N1 swine flu, as that is a strain of flu that is substantially different than seasonal flu, and hence prior exposure to seasonal flu will not protect against H1N1.
 Staphylococcus aureus can cause a bacterial skin infection that can become very serious.
Staphylococcus aureus can cause a bacterial skin infection that can become very serious.
a. Why does the body exhibit innate and adaptive responses to Staphylococcus aureus but not to its own skin cells?
b. Will the innate response to Staphylococcus aureus be equally effective against Streptococcus pyogenes, another bacterium that can cause skin infections? Explain your answer.
c. Will the adaptive response to Staphylococcus aureus be equally effective against Streptococcus pyogenes? Explain your answer.
a: S. aureus is foreign, or nonself. Both innate and adaptive immunity act against foreign invaders. b: Yes. Because the innate response does not specifically recognize individual pathogens, the innate response to S. aureus will be equally effective against S. pyogenes. c: No. The adaptive response to S. aureus will not be effective against S. pyogenes. The adaptive response to S. aureus is specific to S. aureus and is not effective against other bacteria.
 HIV is a virus that infects and eventually destroys helper T cells. Why do people with AIDS (that is, with advanced HIV infections) often die from infections by other pathogens?
HIV is a virus that infects and eventually destroys helper T cells. Why do people with AIDS (that is, with advanced HIV infections) often die from infections by other pathogens?
Helper T cells are critical in mounting an effective adaptive response. In the absence of helper T cells, the ability to mount an adaptive immune response is compromised, leaving someone with AIDS vulnerable to a variety of infections.
MINI CASE
 In 2008, there was an outbreak of measles in San Diego. The first patient was a 7-year-old unvaccinated boy who had returned home from a family trip to Switzerland. He began to develop a cough, sore throat, and fever, but continued to attend school. He was taken to his pediatrician when he developed a rash, and then was sent to the emergency room because of a very high fever. Blood tests revealed antimeasles antibodies. Eleven other children ended up developing measles; none had been vaccinated. The other cases were the 2 siblings of the first patient, 4 children in his school and 5 children who were in the pediatrician’s office at the same time as the patient. Of the 11 additional cases, 3 children were less than 1 year old. (Data are from Outbreak of measles–San Diego, California, January–February 2008. (2008) Morbidity and Mortality Weekly Report 57(8): 203–206.)
In 2008, there was an outbreak of measles in San Diego. The first patient was a 7-year-old unvaccinated boy who had returned home from a family trip to Switzerland. He began to develop a cough, sore throat, and fever, but continued to attend school. He was taken to his pediatrician when he developed a rash, and then was sent to the emergency room because of a very high fever. Blood tests revealed antimeasles antibodies. Eleven other children ended up developing measles; none had been vaccinated. The other cases were the 2 siblings of the first patient, 4 children in his school and 5 children who were in the pediatrician’s office at the same time as the patient. Of the 11 additional cases, 3 children were less than 1 year old. (Data are from Outbreak of measles–San Diego, California, January–February 2008. (2008) Morbidity and Mortality Weekly Report 57(8): 203–206.)
a. Why was the presence of antimeasles antibodies in the first case an important finding?
b. What can you infer about how easily measles spreads?
c. What does this case suggest about the importance of measles vaccinations?
d. Were all the unvaccinated children necessarily behind on their vaccination schedule? (Hint: Look up the recommended measles vaccination schedule on the CDC website www.cdc.gov.)
a: As the boy had not been vaccinated, the only way he would have antimeasles antibodies would be if he had been exposed to the measles virus. This circumstance helped make the diagnosis of measles. b: Children in the doctor’s office and in the school developed measles by simply being in the same place as the patient; this suggests that measles spreads very easily. c: All of the children who developed measles were unvaccinated, suggesting that they are vulnerable to developing measles when unvaccinated. d: The first measles shot should be given around the first birthday, at 12–15 months of age. Thus, the youngest children (those less than a year old) were not behind on their vaccination schedule—they were too young to be vaccinated, and therefore vulnerable to contracting measles.
BRING IT HOME
 Almost 10% of the children in the school attended by the original patient described in the Mini Case were unvaccinated because their parents had filed Personal Belief Exemptions stating that they did not want to vaccinate their children. What is your local school district or state policy on vaccinations for enrolled students? This information is typically available at the school district website or the state’s Department of Health website. From the policies in place (and whether they permit any exemptions), do you think it is possible that a measles outbreak could occur in a local school?
Almost 10% of the children in the school attended by the original patient described in the Mini Case were unvaccinated because their parents had filed Personal Belief Exemptions stating that they did not want to vaccinate their children. What is your local school district or state policy on vaccinations for enrolled students? This information is typically available at the school district website or the state’s Department of Health website. From the policies in place (and whether they permit any exemptions), do you think it is possible that a measles outbreak could occur in a local school?
Answers will vary. Some states allow exemptions for personal beliefs, some allow exemptions for religious reasons, and exemptions can be requested because of allergies to the components of a vaccine. If a substantial proportion of students in a school are unvaccinated, vaccine-preventable diseases such as measles can spread throughout the unvaccinated population.
DRIVING QUESTION 4
What are specific features of influenza virus that allow it to cause worldwide outbreaks?
By answering the questions below and studying Infographics 31.5 and 31.10, you should be able to generate an answer for the broader Driving Question above.
KNOW IT
 What is the difference between antigenic shift and antigenic drift?
What is the difference between antigenic shift and antigenic drift?
Antigenic shift is said to occur when segmented viruses exchange segments, such that a virus can have a genomic segment (and corresponding genes) from a completely different virus. These viruses tend to be very different than either starting virus. “Antigenic drift” describes small changes (caused by mutations) in the viral genome.
 A strain of influenza can infect and replicate in birds without causing them disease. The same strain can be transmitted from birds to humans, causing severe illness in humans. What else would this strain need to be able to do in order to become pandemic?
A strain of influenza can infect and replicate in birds without causing them disease. The same strain can be transmitted from birds to humans, causing severe illness in humans. What else would this strain need to be able to do in order to become pandemic?
To become pandemic, this virus would have to spread easily from human to human, thus spreading widely throughout the human population.
USE IT
 What processes are responsible for the emergence of pandemic influenza strains such as H1N1 swine flu? Explain how these strains can spread so successfully through the human population.
What processes are responsible for the emergence of pandemic influenza strains such as H1N1 swine flu? Explain how these strains can spread so successfully through the human population.
Pandemic viruses typically arise by antigenic shift. When two different viruses (e.g., a pig virus and a human virus) co-infect a single cell, they can swap genomic segments, resulting in new viruses with genes from both of the starting viruses. When these viruses infect humans, the human population does not have immunity against the proteins encoded by the new swine virus segments. This allows them to spread easily throughout the population.
 In 2013, the CDC advised people traveling to China to avoid visiting poultry farms or bird markets. Why did the CDC make this recommendation?
In 2013, the CDC advised people traveling to China to avoid visiting poultry farms or bird markets. Why did the CDC make this recommendation?
A new H7N9 bird flu caused severe illness and deaths in humans in China in 2013. This virus has been detected in poultry in China. By minimizing exposure to poultry markets, people can reduce their chance of exposure to and infection by this new avian flu.
 Why are those with influenza infections susceptible to bacterial pneumonia?
Why are those with influenza infections susceptible to bacterial pneumonia?
Because influenza infections and the inflammatory responses initiated by influenza infections can damage the respiratory tract lining, influenza infections damage one of the first lines of response to other infections, leaving them vulnerable to the entry and infection of pathogenic bacteria.
INTERPRETING DATA
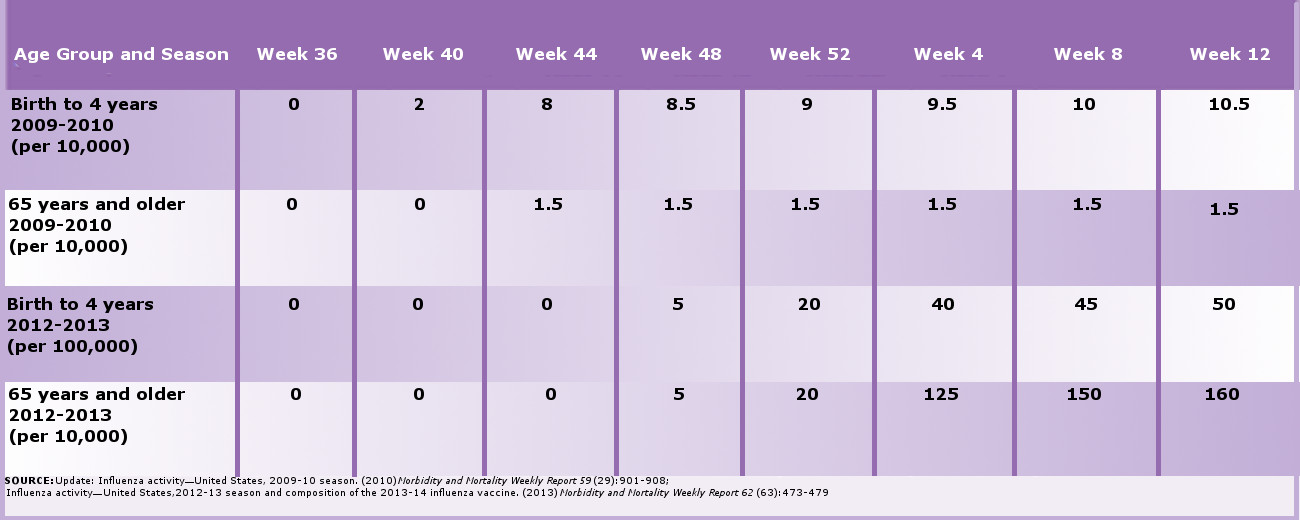
 The table below gives the approximate cumulative rate of influenza hospitalizations in the United States in newborns to 4-year-olds and in people 65 years old and older for the 2009–2010 flu season and the 2012–2013 flu season. As the flu season runs from the fall of one year through the spring of the next, the data are reported by week (36th week of the first year to 12th week of the next).
The table below gives the approximate cumulative rate of influenza hospitalizations in the United States in newborns to 4-year-olds and in people 65 years old and older for the 2009–2010 flu season and the 2012–2013 flu season. As the flu season runs from the fall of one year through the spring of the next, the data are reported by week (36th week of the first year to 12th week of the next).
a. Graph the cumulative incidence rates by week for each age group in each flu season. In plotting the data on the graph, note that the rates in the two seasons are reported differently–per 10,000 and per 100,000–and be sure your graph accounts for this.
b. Examine each season and compare and contrast the age-specific hospitalization rates in the two seasons.
c. Which of the two flu seasons is more typical? Why?
a: Graph not provided in answer key
b: In 2009–2010, the age group from birth to 4 years started being hospitalized earlier, and there were dramatically more hospitalizations in this age group compared to the 65 and older group. This in contrast to 2012–2013, in which there were more hospitalizations in the 65 and older group. There were overall more hospitalizations in the age group from birth to 4 years in 2009–2010.c: The 2012–2013 flu season is more typical, as most of the hospitalizations are occurring in the older population.