15.4 Treatment Effectiveness: For Better or for Worse
Think back to Christine and the dead mouse at the beginning of the chapter. What if, instead of exposure and response prevention, Christine had been assigned psychoanalysis or psychosurgery? Could these alternatives have been just as effective (and justified) for treating her OCD? Throughout this chapter, we have explored various psychological and biological treatments that may help people with psychological disorders. But do these treatments actually work, and which ones work better than the others?
As you learned in the Methods in Psychology chapter, pinning down a specific cause for an effect can be a difficult detective exercise. The detection is made even more difficult because people may approach treatment evaluation very unscientifically, often by simply noticing an improvement (or no improvement) and reaching a conclusion based on that sole observation. Determination of a treatment’s effectiveness can be misdirected by illusions that can only be overcome by careful, scientific evaluation.
Treatment Illusions
Imagine you’re sick and the doctor says, “Take a pill.” You follow the doctor’s orders, and you get better. To what do you attribute your improvement? If you’re like most people, you reach the conclusion that the pill cured you. That’s one possible explanation, but you might have fallen victim to an illusion of treatment. Such illusions can be produced by natural improvement, by placebo effects, and by reconstructive memory. Let’s look more closely at each.
500
1. Natural Improvement
Natural improvement is the tendency of symptoms to return to their mean or average level. The illusion in this case happens when you conclude mistakenly that a treatment has made you better when you would have gotten better anyway. People typically turn to therapy or medication when their symptoms are at their worst. When this is the case, the client’s symptoms will often improve regardless of whether there was any treatment at all; when you’re at rock bottom, there’s nowhere to move but up. In most cases, for example, depression that becomes severe enough to make individuals candidates for treatment will tend to lift in several months no matter what they do. A person who enters therapy for depression may develop an illusion that the therapy works because the therapy coincides with the typical course of the illness and the person’s natural return to health. How can we know if change was caused by the treatment or by natural improvement? As discussed in the Methods in Psychology chapter, we could do an experiment in which we assign half of the people who are depressed to receive treatment and the other half to receive no treatment, and then we could monitor them over time to see if the ones who got treatment actually show greater improvement. This is precisely how researchers test out different interventions, as described in more detail below.
2. Placebo Effects
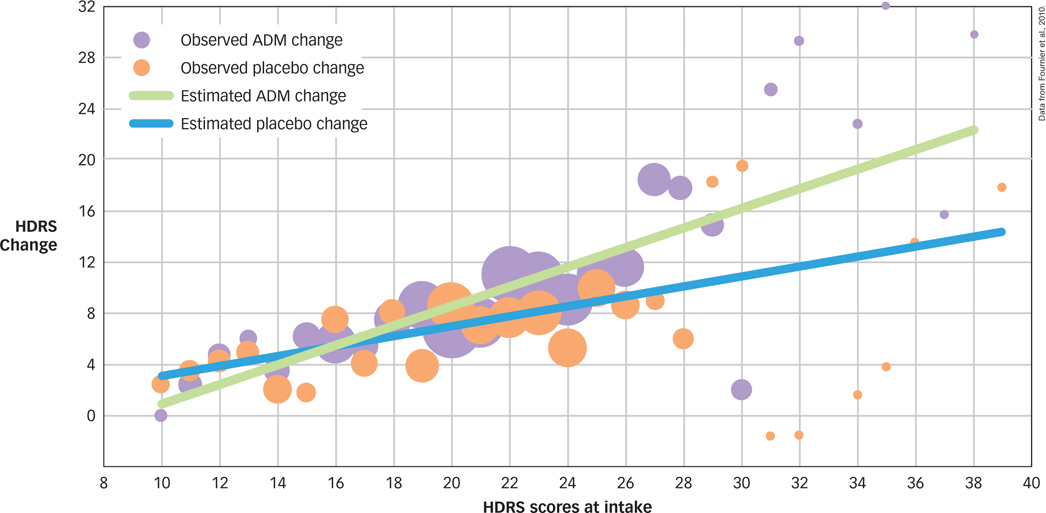
Recovery could be produced by nonspecific treatment effects that are not related to the specific mechanisms by which treatment is supposed to be working. For example, simply knowing that you are getting a treatment can be a nonspecific treatment effect. These instances include the positive influences that can be produced by a placebo, an inert substance or procedure that has been applied with the expectation that a healing response will be produced. Research shows that a large percentage of individuals with anxiety, depression, and other emotional and medical problems experience significant improvement after a placebo treatment. One recent study considered 718 patients with depression who were randomly assigned to receive either antidepressant medication or pill placebo (Fournier et al., 2010). For those participants with mild or moderate depression symptoms, a placebo was just as effective as antidepressant medication, and it was only in instances of severe depression that antidepressants seem to work better than placebos (see FIGURE 15.7).
placebo
An inert substance or procedure that has been applied with the expectation that a healing response will be produced.
What is the placebo effect?
3. Reconstructive Memory
A third treatment illusion can come about when the client’s motivation to get well causes errors in reconstructive memory for the original symptoms. You might think that you’ve improved because of a treatment when in fact you’re simply misremembering: You mistakenly believe that your symptoms before treatment were worse than they actually were. For example, a client who forms a strong expectation of success in therapy might conclude later that even a useless treatment had worked wonders by recalling past symptoms and troubles as worse than they were and thereby making the treatment seem effective.
Treatment Studies
How can we make sure that we are using treatments that actually work and not wasting time with procedures that may be useless or even harmful? Research psychologists use the approaches covered in the Methods in Psychology chapter to create experiments that test whether treatments are effective for the different mental disorders described in the previous chapter.
501
Treatment outcome studies are designed to evaluate whether a particular treatment works, often in relation to some other treatment or a control condition. For example, to study the outcome of treatment for depression, researchers might compare the self-
Researchers use a range of methods to ensure that any observed effects are not due to the treatment illusions described earlier. For example, the treatment illusions caused by natural improvement and reconstructive memory happen when people compare their symptoms before treatment to their symptoms after treatment. To avoid this, a treatment (or experimental) group and a control group need to be randomly assigned to each condition and then compared at the end of treatment. That way, natural improvement or motivated reconstructive memory can’t cause illusions of effective treatment.
Why is a double-
But what should happen to the control group during the treatment? If its members simply stay home, waiting until they can get treatment later (a wait-
502
Which Treatments Work?
The distinguished psychologist Hans Eysenck (1916–
|
Disorder |
Treatment |
Results |
|---|---|---|
|
Depression |
CBT |
PT = meds; PT + meds > either alone |
|
Panic disorder |
CBT |
PT > meds at follow- end of treatment; both > placebo |
|
Posttraumatic stress disorder |
CBT |
PT > present- |
|
Tourette’s disorder |
Habit reversal training |
PT > supportive therapy |
|
Insomnia |
CBT |
PT > medication or placebo |
|
Depression and physical health in Alzheimer’s patients |
Exercise and behavioral management |
PT > routine medical care |
|
Gulf War Veterans’ illnesses |
CBT and exercise |
PT > usual care or alternative treatments |
|
Note: CBT = cognitive behavior therapy; PT = psychological treatment; Meds = medication. Source: Information from Barlow et al., 2013. |
||

Some have questioned whether treatments shown to work in treatment studies conducted at university clinics will work in the real world. For instance, most treatment studies reported in the literature do not have large numbers of participants who are of ethnic minority status, and so it is unclear if these treatments will work with ethnically and culturally diverse groups. One recent, comprehensive review of all available data suggests that although there are gaps in the literature, results suggest that current evidence-
503
Even trickier than the question of establishing whether a treatment works is whether a psychotherapy or medication might actually do harm. The dangers of drug treatment should be clear to anyone who has read a magazine ad for a drug and studied the fine print with its list of side effects, potential drug interactions, and complications. Many drugs used for psychological treatment may be addictive, creating long-
How do psychologists know which treatments work and which might be harmful?
The dangers of psychotherapy are more subtle, but one is clear enough in some cases that there is actually a name for it. Iatrogenic illness is a disorder or symptom that occurs as a result of a medical or psychotherapeutic treatment itself (e.g., Boisvert & Faust, 2002). Such an illness might arise, for example, when a psychotherapist becomes convinced that a client has a disorder that in fact the client does not have. As a result, the therapist works to help the client accept that diagnosis and participate in psychotherapy to treat that disorder. Being treated for a disorder can, under certain conditions, make a person show signs of that very disorder—
iatrogenic illness
A disorder or symptom that occurs as a result of a medical or psychotherapeutic treatment itself.
Just as psychologists have created lists of treatments that work, they also have begun to establish lists of treatments that harm. The purpose of doing so is to inform other researchers, clinicians, and the public which treatments they should avoid. Many are under the impression that although every psychological treatment may not be effective, some treatment is better than no treatment. However, it turns out that a number of interventions intended to help alleviate people’s symptoms actually make them worse! Did your high school have a D.A.R.E. (Drug Abuse and Resistance Education) program? Have you heard of critical-
|
Type of Treatment |
Potential Harm |
Source of Evidence |
|---|---|---|
|
CISD |
Increased risk of PTSD |
RCTs |
|
Scared straight |
Worsening of conduct problems |
RCTs |
|
Boot- |
Worsening of conduct problems |
Meta- |
|
D.A.R.E. programs |
Increased use of alcohol and drugs |
RCTs |
|
Note: CISD = critical- Source: Information from Lilienfeld, 2007. |
||
To regulate the potentially powerful influence of therapies, psychologists hold themselves to a set of ethical standards for the treatment of people with mental disorders (American Psychological Association, 2002). Adherence to these standards is required for membership in the American Psychological Association, and state licensing boards also monitor adherence to ethical principles in therapy. These ethical standards include (a) striving to benefit clients and taking care to do no harm; (b) establishing relationships of trust with clients; (c) promoting accuracy, honesty, and truthfulness; (d) seeking fairness in treatment and taking precautions to avoid biases; and (e) respecting the dignity and worth of all people. When people suffering from mental disorders come to psychologists for help, adhering to these guidelines is the least that psychologists can do. Ideally, in the hope of relieving this suffering, they can do much more.
504
SUMMARY QUIZ [15.4]
Question 15.10
| 1. | Which treatment illusion occurs when a client or therapist attributes the client’s improvement to a feature of treatment, although that feature wasn’t really the active element that caused improvement? |
- nonspecific treatment effects
- natural improvement
- error in reconstructive memory
- regression to the mean
a.
Question 15.11
| 2. | Current studies indicate that the typical psychotherapy client is better off than __________________ of untreated individuals. |
- one half
- the same number
- one fourth
- three fourths
d.