10.3 The Treatment of Mental Disorders
Before discussing treatment for disorders (types of therapy), we need to describe the various types of mental health professionals who treat disorders. Table 10.3 lists most of the major types of mental health professionals, along with the type of credential and the typical kinds of problems they treat. States have licensing requirements for these various mental health professionals, and it is important to verify that a therapist is licensed. There is also one major difference between psychiatrists and the other health professionals. Psychiatrists are medical doctors. This means that psychiatrists can write prescriptions for medical treatment of patients. This is especially important because drug therapy is the major type of treatment for many disorders. To circumvent this prescription-
| Type | Credential and Job Description |
|---|---|
| Clinical psychologist | Doctoral degree in clinical psychology; provides therapy for people with mental disorders |
| Counseling psychologist | Doctoral degree in psychological or educational counseling; counsels people with milder problems such as academic, job, and relationship problems |
| Psychiatrist | Medical degree with residency in mental health; provides therapy for people with mental disorders and is the only type of therapist who can prescribe drugs or other biomedical treatment |
| Psychoanalyst | Any of the above types of credential, but with training in psychoanalysis from a psychoanalytic institute; provides psychoanalytic therapy for psychological disorders |
| Clinical social worker | Master’s or doctoral degree in social work with specialized training in counseling; provides help with social problems, such as family problems |
biomedical therapy The use of biological interventions, such as drugs, to treat mental disorders.
psychotherapy The use of psychological interventions to treat mental disorders.
There are two major types of therapy: biomedical and psychological. Biomedical therapy involves the use of biological interventions, such as drugs, to treat disorders. Psychotherapy involves the use of psychological interventions to treat disorders. Psychotherapy is what we normally think of as therapy. There is a dialogue and interaction between the person and the therapist. They talk to each other. This is why psychotherapy is sometimes referred to as “talk therapy.” The nature of the “talk” varies with the approach of the therapist. The behavioral, cognitive, psychoanalytic, and humanistic approaches all lead to different styles of psychotherapy. In biomedical therapy, however, a drug or some other type of biological intervention is used to treat disorders. The interaction is biological, not interpersonal. As with psychotherapy, there are different types of biomedical therapy—
Biomedical Therapies
Biomedical therapies for disorders have a long history, reaching back hundreds of years. Looking back, these earlier treatments may seem inhumane and cruel, but remember that we are assessing these treatments given our current state of medical and psychological knowledge, which is far superior to that available when such treatments were used. Let’s consider a couple of examples.
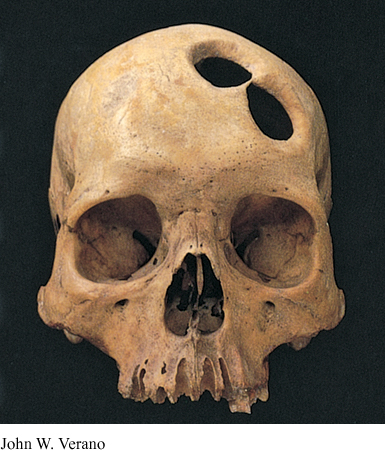
Possibly the earliest biological treatment was trephining, which was done in the Middle Ages. In this primitive treatment, a trephine (stone tool) was used to cut away a section of the person’s skull, supposedly to let evil spirits exit the body, thus freeing the person from the disorder. A treatment device from the early 1800s was called the “tranquilizing chair.” This device was designed by Benjamin Rush, the “father of American psychiatry,” who actually instituted many humane reforms in the treatment of mental patients (Gamwell & Tomes, 1995). The treatment called for patients to be strapped into a tranquilizing chair, with the head enclosed inside a box, for long periods of time. The restriction of activity and stimulation was supposed to have a calming effect by restricting the flow of blood to the patient’s brain. Such “therapies” seem absurd to us today, as does the fact that well into the nineteenth century, many mental patients were still being kept in chains in asylums, untreated. The history of therapy is a rather sad one.

Even the more contemporary biomedical treatments exist in an atmosphere of controversy. Most people have strong, negative feelings about shock therapy, and the most frequently used biomedical treatment, drug therapy, is shrouded in conflict (Barber, 2008; Moncrieff, 2009; Valenstein, 1988). Why? Biomedical treatments are very different from undergoing psychotherapy. Direct biological interventions have a more powerful downside, because they involve possibly serious medical side effects. For example, high levels of some drugs in the blood are toxic and may even be fatal. Careful monitoring is essential. As we discuss the major types of biomedical treatments, we will include discussion of some of these potential problems. We start with drug therapy.
Drug therapy. The drugs used to treat mental disorders are referred to as psychotropic drugs, and they are among the very best sellers for drug companies, with about 300 million prescriptions written for them yearly in the United States (Frances, 2013). Leading the way are antipsychotic drugs with sales of $18 billion a year and antidepressant drugs with sales of $12 billion a year. Surprisingly, primary care providers, not psychiatrists, write the majority of these prescriptions (DuBosar, 2009). In addition to antipsychotic and antidepressant drugs, other major psychotropic medications used in drug therapy are antianxiety drugs and lithium. We will discuss all of these, beginning with lithium.
lithium A naturally occurring element (a mineral salt) that is used to treat bipolar disorder.
Lithium is not a drug, but rather a naturally occurring metallic element (a mineral salt) that is used to treat bipolar disorder. Lithium was actually sold as a substitute for table salt in the 1940s and was added to some commercial drinks, such as 7-
antidepressant drugs Drugs used to treat depressive disorders.
Antidepressant drugs are drugs used to treat depressive disorders. There are many different types. The first antidepressants developed were monoamine oxidase (MAO) inhibitors and tricyclics (this name refers to the three-
Research indicates that MAO inhibitors are fairly successful in combating depressive symptoms, but they are not used very often because of a potentially very dangerous side effect. Their interaction with several different foods and drinks may result in fatally high blood pressure. Tricyclics are prescribed more often than MAO inhibitors, because they are not subject to this potentially dangerous interaction. The most prescribed antidepressants by far, however, are the more recently developed selective serotonin reuptake inhibitors (SSRIs). Remember from Chapter 2 that their name describes how they achieve their effect—
A recent survey study of about 12,000 people by the Centers for Disease Control and Prevention found some interesting results with respect to the use of antidepressants (Pratt, Brody, & Gu, 2011). First, the use of antidepressant drugs has soared nearly 400% since 1988, making antidepressants the most frequently used drugs by people ages 18–
There is a controversy about the effectiveness of antidepressant drugs, with some researchers arguing that antidepressants are just expensive, overused placebos. Indeed, some recent research indicates that much of their effectiveness can be accounted for by placebo effects—
neurogenesis theory of depression An explanation of depression that proposes that neurogenesis, the growth of new neurons, in the hippocampus stops during depression, and when it resumes, the depression lifts.
How can we make sense of these placebo effects? One possibility involves neurogenesis, which we discussed in Chapter 2. Remember, neurogenesis, the growth of new neurons, has been observed in the hippocampus in the adult brain (Jacobs, van Praag, & Gage, 2000a, 2000b). The neurogenesis theory of depression assumes that neurogenesis in the hippocampus stops during depression, and when neurogenesis resumes, the depression lifts (Jacobs, 2004). The question, then, is how do we get neurogenesis to resume? There are many possibilities. Research has shown that SSRIs lead to increased neurogenesis in other animals. Both rats and monkeys given Prozac make more neurons than rats and monkeys not given Prozac (Perera et al., 2011). This also seems to be the case for humans taking antidepressants (Boldrini et al., 2009; Malberg & Schechter, 2005). The time frame for neurogenesis also fits the time frame for SSRIs to have an impact on mood. It takes 3 to 6 weeks for new cells to mature, the same time it typically takes SSRIs to improve the mood of a patient. This means that, in the case of the SSRIs, the increased serotonin activity may be responsible for getting neurogenesis going again and lifting mood.
Remember, however, what we said about disorders being biopsychosocial phenomena. It is certainly plausible that psychological factors could also have an impact on neurogenesis. Positive thinking, in the form of a strong placebo effect, might also get neurogenesis going again, but possibly not sufficiently enough to deal with very severe depression. A similar claim could be made for the effectiveness of cognitive psychotherapies in which therapists turn the patient’s negative thinking into more positive thinking. The neurogenesis theory is only in its formative stage, but it does provide a coherent framework for the many diverse improvement effects due to drugs, placebos, and psychotherapies.
antianxiety drugs Drugs used to treat anxiety problems and disorders.
Antianxiety drugs are drugs that treat anxiety problems and disorders. The best known antianxiety drugs, such as Valium and Xanax, are in a class of drugs called benzodiazepines. Benzodiazepines reduce anxiety by increasing the activity of the major inhibitory neurotransmitter GABA. They achieve their agonistic effect by facilitating GABA binding at GABA receptors (Advokat et al., 2014). When GABA’s activity is increased, it reduces anxiety by slowing down and inhibiting neural activity, getting it back to normal levels. Unfortunately, recent evidence has shown that benzodiazepines have potentially dangerous side effects, such as physical dependence or fatal interactions with alcohol, but other types of nonbenzodiazepine antianxiety drugs have been developed with milder side effects. In addition, some antidepressant drugs, especially the SSRIs, have been very successful in treating anxiety disorders.
antipsychotic drugs Drugs used to treat psychotic disorders.
Antipsychotic drugs are drugs that reduce psychotic symptoms. The first antipsychotic drugs appeared in the 1950s and, as we discussed in Chapter 2, worked antagonistically by globally blocking receptor sites for dopamine, thereby reducing its activity. These drugs greatly reduced the positive symptoms of schizophrenia but had little impact on the negative symptoms. Antipsychotic drugs revolutionized the treatment of schizophrenia and greatly reduced the number of people with schizophrenia in mental institutions. These early drugs, along with those developed through the 1980s, are referred to as “traditional” antipsychotic drugs to distinguish them from the more recently developed “new generation” antipsychotic drugs.
tardive dyskinesia A side effect of long-
The traditional drugs (for example, Thorazine and Stelazine) produce side effects in motor movement that are similar to the movement problems of Parkinson’s disease. In addition, there is a long-
Regrettably, the new generation antipsychotic drugs have other potentially dangerous side effects and have to be monitored very carefully (Folsom, Fleisher, & Depp, 2006). Such monitoring is expensive; therefore, traditional drugs are often prescribed instead. In addition, the initial optimism for the new generation drugs has been tempered by recent evidence that they do not lead to as much improvement as originally thought (Jones et al., 2006; Lieberman, Stroup, et al., 2005). A recent study of long-
A different type of new generation antipsychotic drug, trade name Abilify, is sometimes referred to as a “third generation” antipsychotic drug because of its neurochemical actions. It achieves its effects by stabilizing the levels of both dopamine and serotonin activity in certain areas of the brain. It blocks receptor sites for these two neurotransmitters when their activity levels are too high and stimulates these receptor sites when their activity levels are too low. Thus, it works in both antagonistic and agonistic ways, depending upon what type of effect is needed. This is why it is also sometimes called a “dopamine-

electroconvulsive therapy (ECT) A biomedical treatment for severe depression that involves electrically inducing a brief brain seizure.
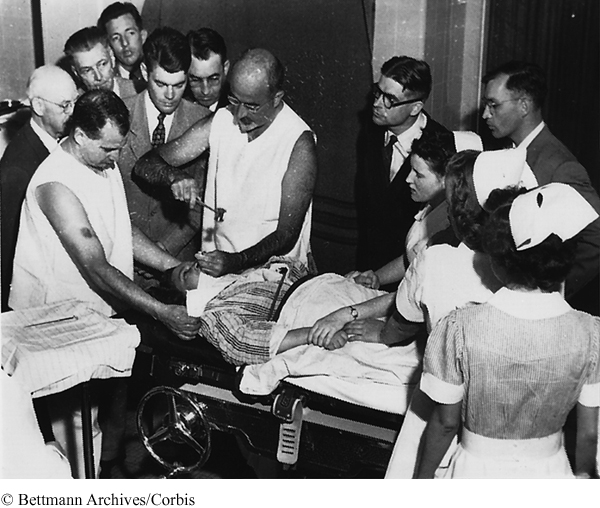
Electroconvulsive therapy. Another type of biomedical therapy is electroconvulsive therapy (ECT), a last-

About 80% of depressed patients improve with ECT (Glass, 2001), and they show improvement somewhat more rapidly with the use of ECT than with antidepressant drugs (Seligman, 1994). This more rapid effect makes ECT a valuable treatment for suicidal, severely depressed patients, especially those who have not responded to any other type of treatment. Strangely, after more than 50 years we still do not know how ECT works in treating depression. One explanation is that, like antidepressant drugs, the electric shock increases the activity of serotonin and norepinephrine, which improves mood. ECT’s effects also fit the speculative neurogenesis theory of depression. Like SSRIs, electroconvulsive shock increases neurogenesis in rats (Scott, Wojtowicz, & Burnham, 2000). This means that ECT may have an impact on neurogenesis and may do so a little more quickly than antidepressant drugs. Current research seems to indicate that ECT does not lead to any type of detectable brain damage or long-
transcranial magnetic stimulation (TMS) A neurostimulation therapy in which the left frontal lobe is stimulated with magnetic pulses via an electromagnetic coil placed on the patient’s scalp. It is only cleared for use in cases of severe depression for which traditional treatment has not helped.
Because of the general public’s negative image of ECT, alternative neurostimulation therapies for the severely depressed are being developed. One promising alternative is transcranial magnetic stimulation (TMS). In contrast with ECT, which transmits electrical impulses, TMS stimulates the brain with magnetic pulses via an electromagnetic coil placed on the patient’s scalp above the left frontal lobe. This area is stimulated because brain scans of depressed patients show that it is relatively inactive. Typically a patient receives five treatments a week for 4 to 6 weeks. Unlike ECT, the patient is awake during TMS, and TMS does not produce any memory loss or other major side effects. Like ECT, it is not exactly clear how TMS works to alleviate depression, but it seems to do so by energizing neuronal activity in a depressed patient’s relatively inactive left frontal lobe. Although some research has shown that it may be as effective as ECT in treating severely depressed patients for whom more traditional treatments have not helped (Grunhaus, Schreiber, Dolberg, Polak, & Dannon, 2003) and its use for this purpose has been approved, more research on this relatively new therapy and its effects is clearly needed.
psychosurgery A biomedical treatment in which specific areas of the brain are destroyed.
lobotomy A type of psychosurgery in which the neuronal connections of the frontal lobes to lower brain areas are severed.
Psychosurgery. An even more controversial biomedical therapy is psychosurgery, the destruction of specific areas in the brain. The most famous type of psychosurgery is the lobotomy, in which the neuronal connections of the frontal lobes to lower areas in the brain are severed. Egas Moniz, a Portuguese neurosurgeon who coined the term “psychosurgery,” pioneered work on lobotomies for the treatment of schizophrenia (Valenstein, 1986). In fact, he won a Nobel Prize for Medicine in 1949 for his work. However, not everything went well for Moniz. Ten years earlier, he was almost killed by one of his patients—
Psychosurgery is still around, but it is very different from the earlier primitive lobotomies (Vertosick, 1997). For example, cingulotomies, in which dime-
Psychotherapies
In Chapter 8, one type of psychotherapy, psychoanalysis, developed by Sigmund Freud in the early 1900s, was briefly discussed. When thinking about psychoanalysis, we usually think of a patient lying on a couch with the therapist sitting behind the patient and taking notes about the patient’s dreams and free associations. This is actually a fairly accurate description of classical psychoanalysis, but most types of psychotherapy are nothing like this. We’ll discuss psychoanalysis first and then the other three major types of psychotherapy—
psychoanalysis A style of psychotherapy, originally developed by Sigmund Freud, in which the therapist helps the person gain insight into the unconscious sources of his or her problems.
Psychoanalysis. Psychoanalysis is a style of psychotherapy, originally developed by Sigmund Freud, in which the therapist helps the person gain insight into the unconscious sources of his or her problems. Classical psychoanalysis, as developed by Freud, is very expensive and time consuming. A patient usually needs multiple sessions each week for a year or two to get to the source of her problems. Remember from Chapter 8 that Freud proposed that problems arise from repressed memories, fixations, and unresolved conflicts, mainly from early childhood. Such problems are repressed in the unconscious but continue to influence the person’s behavior and thinking. The task for the psychoanalyst is to discover these underlying unconscious problems and then help the patient to gain insight into them. The difficulty with this is that the patient herself is not even privy to these unconscious problems. This means that the therapist has to identify conscious reflections of the underlying problems and interpret them. The major task of the psychoanalyst, then, is to interpret many sources of input—
free association A person spontaneously describes, without editing, all thoughts, feelings, or images that come to mind.
resistance A person’s unwillingness to discuss a particular topic during therapy.
Free association is a technique in which the patient spontaneously describes, without editing, all thoughts, feelings, or images that come to mind. For psychoanalysts, free association is like a verbal projective test. Psychoanalysts assume that free association does not just produce random thoughts but will provide clues to the unconscious conflicts leading to the patient’s problems. This is especially true for resistances during free association. A resistance is a patient’s unwillingness to discuss particular topics. For example, a patient might be free associating and say the word “mother.” A resistance to this topic (his mother) would be indicated by the patient abruptly halting the association process and falling silent. The patient might also miss a therapy appointment to avoid talking about a particular topic (such as his mother) or change the subject to avoid discussion of the topic. The psychoanalyst must detect these resistances and interpret them.
manifest content Freud’s term for the literal surface meaning of a dream.
latent content Freud’s term for the underlying true meaning of a dream.
transference When a person undergoing therapy acts toward the therapist as he or she did or does toward important figures in his or her life, such as his or her parents.
The psychoanalyst also interprets the patient’s dreams, which may provide clues to the underlying problem. According to Freud, psychological defenses are lowered during sleep; therefore, the unconscious conflicts are revealed symbolically in one’s dreams. This means that dreams have two levels of meaning—
Classical psychoanalysis requires a lot of time, because the therapist has to use these various indirect clues to build an interpretation of the patient’s problem. It’s similar to a detective trying to solve a case without any solid clues, such as the weapon, fingerprints, or DNA evidence. There’s only vague circumstantial evidence. Using this evidence, the therapist builds an interpretation that helps the patient to gain insight into the problem. This classical style of psychoanalysis has been strongly criticized and has little empirical evidence supporting its efficacy. However, contemporary psychoanalytic therapy, usually referred to as psychodynamic therapy, has proved successful (Shedler, 2010). It is very different from Freud’s psychoanalysis. The patient sits in a chair instead of lying on a couch, sessions are only once or twice a week, and the therapy may finish in months, instead of years. In addition, patients who receive psychodynamic therapy seem to maintain their therapeutic gains and continue to improve after the therapy ends.
client-
Client-
These conditions are exactly the same as those for healthy personality growth that were discussed in Chapter 8. The therapist should be accepting, genuine, and empathic. The therapist establishes an environment of acceptance by giving the client unconditional positive regard (accepting the client without any conditions upon his behavior). The therapist demonstrates genuineness by honestly sharing her own thoughts and feelings with the client. To achieve empathic understanding of the client’s feelings, the therapist uses active listening to gain a sense of the client’s feelings, and then uses mirroring to echo these feelings back to the client, so that the client can then get a clearer image of his true feelings. It is this realization of his true feelings that allows the client to get back on the road to personal growth and self-
behavioral therapy A style of psychotherapy in which the therapist uses the principles of classical and operant conditioning to change the person’s behavior from maladaptive to adaptive.
Behavioral therapy. Behavioral therapy is a style of psychotherapy in which the therapist uses the principles of classical and operant conditioning to change the person’s behavior from maladaptive to adaptive. The assumption is that the behavioral symptoms (such as the irrational behavior of the woman with the specific phobia of birds) are the problem. Maladaptive behaviors have been learned, so they have to be unlearned, and more adaptive behaviors need to be learned instead. Behavioral therapies are based on either classical or operant conditioning. We’ll first describe an example of one based on classical conditioning.
counterconditioning A type of behavioral therapy in which a maladaptive response is replaced by an incompatible adaptive response.
Remember the Little Albert classical conditioning study by Watson and Rayner that we mentioned earlier in this chapter when we were discussing phobic disorders. As we pointed out in Chapter 4, Albert’s fear of white rats was never deconditioned, but one of Watson’s former students, Mary Cover Jones, later showed that such a fear could be unlearned and replaced with a more adaptive relaxation response (Jones, 1924). Jones eliminated the fear of rabbits in a 3-
systematic desensitization A counterconditioning exposure therapy in which a fear response to an object or situation is replaced with a relaxation response in a series of progressively increasing fear-
Using Jones’s idea that fear and relaxation are incompatible responses, Joseph Wolpe developed a behavioral therapy called systematic desensitization that is very effective in treating phobias (Wolpe, 1958). Systematic desensitization is a counterconditioning procedure in which a fear response to an object or situation is replaced with a relaxation response in a series of progressively increasing fear-
Once the hierarchy is set, the patient is then taught how to use various techniques to relax. Once this relaxation training is over, the therapy begins. The patient starts working through the hierarchy and attempts to relax at each step. First the patient relaxes in imagined situations in the hierarchy and later in the actual situations. With both imagined and actual situations, the anxiety level of the situation is increased slowly. At some of the later stages in the hierarchy, a model of the same sex and roughly same age may be brought in to demonstrate the behavior before the patient attempts it. For example, the model will touch the picture of a bird in a book before the patient is asked to do so. In brief, systematic desensitization teaches the patient to confront progressively increasing fear-
virtual reality therapy A counterconditioning exposure therapy in which the patient is exposed in graduated steps to computer simulations of a feared object or situation.
Virtual reality therapy is similar to systematic desensitization, but the patient is exposed to computer simulations of his fears in a progressively anxiety-
flooding A counterconditioning exposure therapy in which the patient is immediately exposed to a feared object or situation.
Another counterconditioning exposure therapy, flooding, does not involve such gradual confrontation. In flooding, the patient is immediately exposed to the feared object or situation. For example, in the case of the spider phobia, the person would immediately have to confront live spiders. Flooding is often used instead of systematic desensitization when the fear is so strong that the person is unable to make much progress in systematic desensitization.
Behavioral therapies using operant conditioning principles reinforce desired behaviors and extinguish undesired behaviors. A good example is the token economy that we discussed in Chapter 4. A token economy is an environment in which desired behaviors are reinforced with tokens (secondary reinforcers such as gold stars or stickers) that can be exchanged for rewards such as candy and television privileges. This technique is often used with groups of institutionalized people, such as those in mental health facilities. As such, it has been fairly successful in managing populations of people with autism spectrum disorder, intellectual disabilities, and schizophrenia. For example, if making one’s bed is the desired behavior, it will be reinforced with tokens that can be exchanged for treats or privileges. A token economy is more of a way to manage the daily behavior of such people than a way to cure them, but we must remember that a behavioral therapist thinks that the maladaptive behavior is the problem.
cognitive therapy A style of psychotherapy in which the therapist attempts to change the person’s thinking from maladaptive to adaptive.
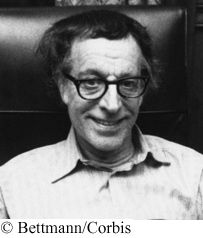
Cognitive therapy. Behavioral therapies work to change the person’s behavior; cognitive therapies work on the person’s thinking. Cognitive therapy is a style of psychotherapy in which the therapist changes the person’s thinking from maladaptive to adaptive. The assumption is that the person’s thought processes and beliefs are maladaptive and need to change. The cognitive therapist identifies the irrational thoughts and unrealistic beliefs that need to change and then helps the person to execute that change. Two prominent cognitive therapies are Albert Ellis’s rational-
rational-
In Ellis’s rational-
Beck’s cognitive therapy A type of cognitive therapy, developed by Aaron Beck, in which the therapist works to develop a warm relationship with the person and has the person carefully consider the evidence for his or her beliefs in order to see the errors in his or her thinking.
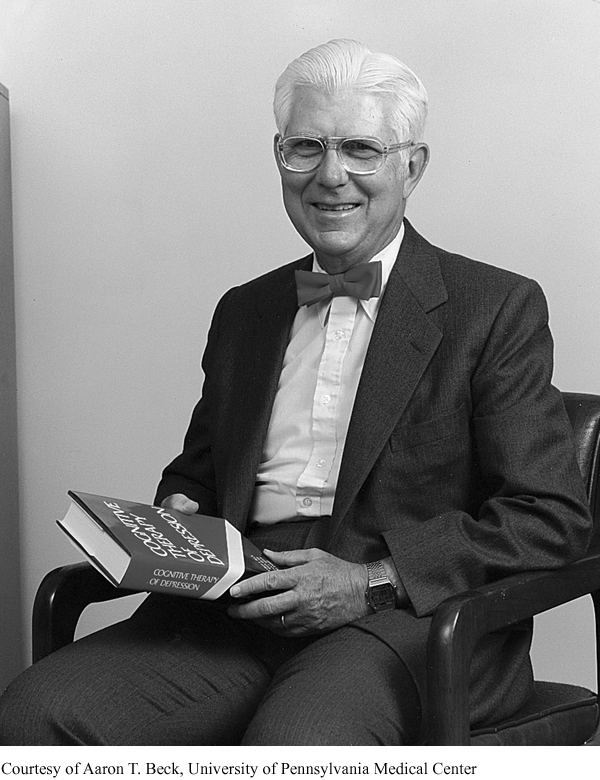
Rational-
spontaneous remission Getting better with the passage of time without receiving any therapy.
Is psychotherapy effective? Now that you understand the four major approaches to psychotherapy, let’s consider the question of whether it is effective or not. To assess the effectiveness of psychotherapy we must consider spontaneous remission, the tincture of time. Spontaneous remission is when a person gets better with the passage of time without receiving any therapy. Thus, spontaneous remission accounts for all of the factors that might lead to improvement other than receiving therapy. One such factor, for example, is regression toward the mean, which we discussed in Chapter 1. Extreme (disordered) behavior and thinking should be followed by more normal behavior and thinking. Another factor would be the beneficial effect of the support of family and friends, a type of informal therapy. And so on. In order to be considered effective then, improvement from psychotherapy must be significantly (statistically) greater than that due to spontaneous remission. To answer the question, researchers have used meta-
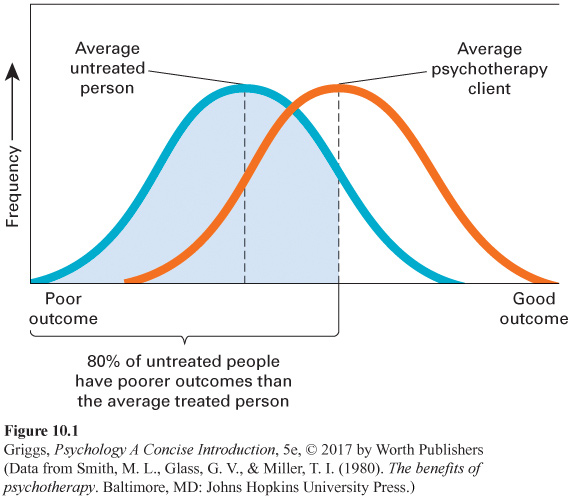
No one particular type of psychotherapy is superior to all of the others. Some types of psychotherapy do, however, seem to be more effective in treating particular disorders. For example, behavioral therapies have been very successful in treating phobias and other anxiety disorders. Also, cognitive therapies tend to be very effective in treating depressive disorders. None of the psychotherapies, however, have been very successful in treating schizophrenia, but, as mentioned earlier in the chapter, some recent findings indicate that combining hybrid cognitive–
Section Summary
There are two major categories of therapy: biomedical and psychological. Biomedical therapy involves the use of biological interventions, such as drugs, to treat disorders. Psychotherapy involves the use of psychological interventions to treat disorders. Psychotherapy is what we normally think of as therapy. In psychotherapy, there is an interaction between the person and the therapist. In biomedical therapy, the interaction is biological. There are three major types of biomedical therapy—
The major medications are lithium, antidepressant drugs, antianxiety drugs, and antipsychotic drugs. Lithium, a naturally occurring mineral salt, is the main treatment for bipolar disorder. There are four types of antidepressants—
There are two types of antipsychotic drugs—
Electroconvulsive therapy (ECT) that involves electrically inducing a brief brain seizure is used almost exclusively to treat severe depression. We do not know how or why this therapy works, but it is a valuable treatment for severely depressed people who have not responded to other types of treatment because it leads to somewhat faster improvement than antidepressant drugs. Given its nature, however, ECT remains shrouded in controversy. An alternative neurostimulation therapy for the severely depressed, transcranial magnetic stimulation (TMS), is not as controversial as ECT and does not produce any major side effects, but more research on its effectiveness is needed.
Even more controversial is psychosurgery, in which specific areas in the brain are actually destroyed. The most famous type of psychosurgery is the lobotomy, in which the neuronal connections of the frontal lobes to lower areas in the brain are severed. No good evidence for why such operations should work or that they did was ever put forth. The arrival of antipsychotic drugs in the 1950s replaced the lobotomy as the main treatment for schizophrenia. Psychosurgery is still around, but it is very different from what it once was and is used very infrequently, only when all other treatments have failed.
Psychotherapies can be categorized into two types—
The most influential humanistic therapy is Rogers’s client-
In behavioral therapies, the therapist uses the principles of classical and operant conditioning to change the person’s behavior from maladaptive to adaptive. The assumption is that the behavioral symptoms are the problem. These behaviors were learned; therefore, they need to be unlearned and more adaptive behaviors learned. Counterconditioning exposure therapies, such as systematic desensitization, virtual reality therapy, and flooding, have been especially effective in treating anxiety disorders such as phobias. Instead of changing the person’s behavior, the cognitive therapist attempts to change the person’s thinking from maladaptive to adaptive. Two major kinds of cognitive therapy are Ellis’s rational-
Using meta-
3
Question 10.7
.
Explain the difference between biomedical therapy and psychotherapy.
In biomedical therapy, there is a direct biological intervention, via drugs or ECT, which has an impact on the biochemistry of the nervous system, or psychosurgery, in which part of the brain is actually destroyed. There is no direct impact on the client’s biology in psychotherapy. Psychological interventions (talk therapies) are used to treat disorders. However, successful psychotherapy may indirectly lead to biological changes in the client’s neurochemistry through more positive thinking.
Question 10.8
.
Explain how the neurogenesis theory of depression could be considered a biopsychosocial explanation.
The neurogenesis theory of depression can be considered a biopsychosocial explanation, because both biological and psychological factors can have an impact on the neurogenesis process that is assumed to eliminate the depression. Antidepressant drugs with their antagonistic effects on serotonin and norepinephrine are good examples of possible biological factors, and the positive thinking produced by cognitive psychotherapy is a good example of a psychological factor.
Question 10.9
.
Explain why the psychoanalyst can be thought of as a detective.
A psychoanalyst can be thought of as a detective, because she has to interpret many clues to the client’s problem. Discovering the client’s problem is like solving a case. The sources of the psychoanalyst’s clues are free association data, resistances, dream analysis, and transferences. The therapist uses these clues to interpret the person’s problem (solve the case) and then uses this interpretation to help the person gain insight into the source of his problem.
Question 10.10
.
Explain the difference between behavioral therapy and cognitive therapy.
Both of these types of psychotherapies are very direct in their approach. However, behavioral therapies assume that the client’s behavior is maladaptive and needs to be replaced with more adaptive behavior. Cognitive therapies instead hold that the client’s thinking is maladaptive and needs to be replaced with more adaptive thinking. In brief, the behavioral therapist works to change the client’s behavior, and the cognitive therapist works to change the client’s thinking.
Question 10.11
.
Explain why a control for spontaneous remission must be included in any assessment of the effectiveness of psychotherapy.
Spontaneous remission is when a person gets better with the passage of time without receiving any therapy. Thus, if it were not considered when the effectiveness of psychotherapy is being evaluated, the researcher might incorrectly assume that the improvement was due to the psychotherapy and not to spontaneous remission. This is why the improvement in wellness for the psychotherapy group must be significantly (statistically) greater than the improvement for the spontaneous remission control group. If it is, then the psychotherapy has produced improvement that cannot be due to just spontaneous remission.