5-3 Neurotransmitter Systems and Behavior
When researchers began to study neurotransmission, they reasoned that any given neuron would contain only one transmitter at all its axon terminals. Newer methods of analysis revealed that this hypothesis isn’t strictly accurate. A single neuron may use one transmitter at one synapse and a different transmitter at another synapse. Moreover, different transmitters may coexist in the same terminal or synapse. Neuropeptides have been found to coexist in terminals with small-
All these findings allow for multiple combinations of neurotransmitters and receptors for them. They caution as well against assuming a simple cause-
We now consider some links between neurotransmitters and behavior. We begin by exploring the three peripheral nervous system divisions: SNS, ANS, and ENS. Then we investigate neurotransmission in the central nervous system.
Neurotransmission in the Somatic Nervous System
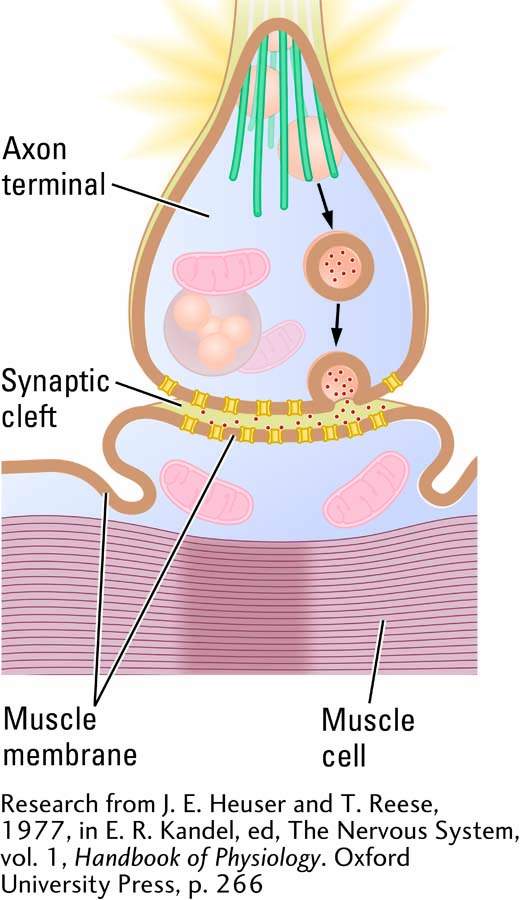
Motor neurons in the brain and spinal cord send their axons to the body’s skeletal muscles, including the muscles of the eyes and face, trunk, limbs, fingers, and toes. Without these SNS neurons, movement would not be possible. Motor neurons are also called cholinergic neurons because acetylcholine is their main neurotransmitter. At a skeletal muscle, cholinergic neurons are excitatory, producing muscular contractions.
Just as a single main neurotransmitter serves the SNS, so does a single main receptor, a transmitter-
Acetylcholine is the primary neurotransmitter at skeletal muscles, but other neurotransmitters also occupy these cholinergic axon terminals and are released onto the muscle along with ACh. One is a neuropeptide called calcitonin gene–
Dual Activating Systems of the Autonomic Nervous System
The complementary ANS divisions, sympathetic and parasympathetic, regulate the body’s internal environment. The sympathetic division rouses the body for action, producing the fight-
Figure 5-16 shows the neurochemical organization of the ANS. Both divisions are controlled by acetylcholine neurons that emanate from the CNS at two levels of the spinal cord. The CNS neurons synapse with parasympathetic neurons that also contain acetylcholine and with sympathetic neurons that contain norepinephrine. In other words, cholinergic neurons in the CNS synapse with sympathetic NE neurons to prepare the body’s organs for fight or flight. Cholinergic neurons in the CNS synapse with autonomic ACh neurons in the parasympathetic division to prepare the body’s organs to rest and digest.
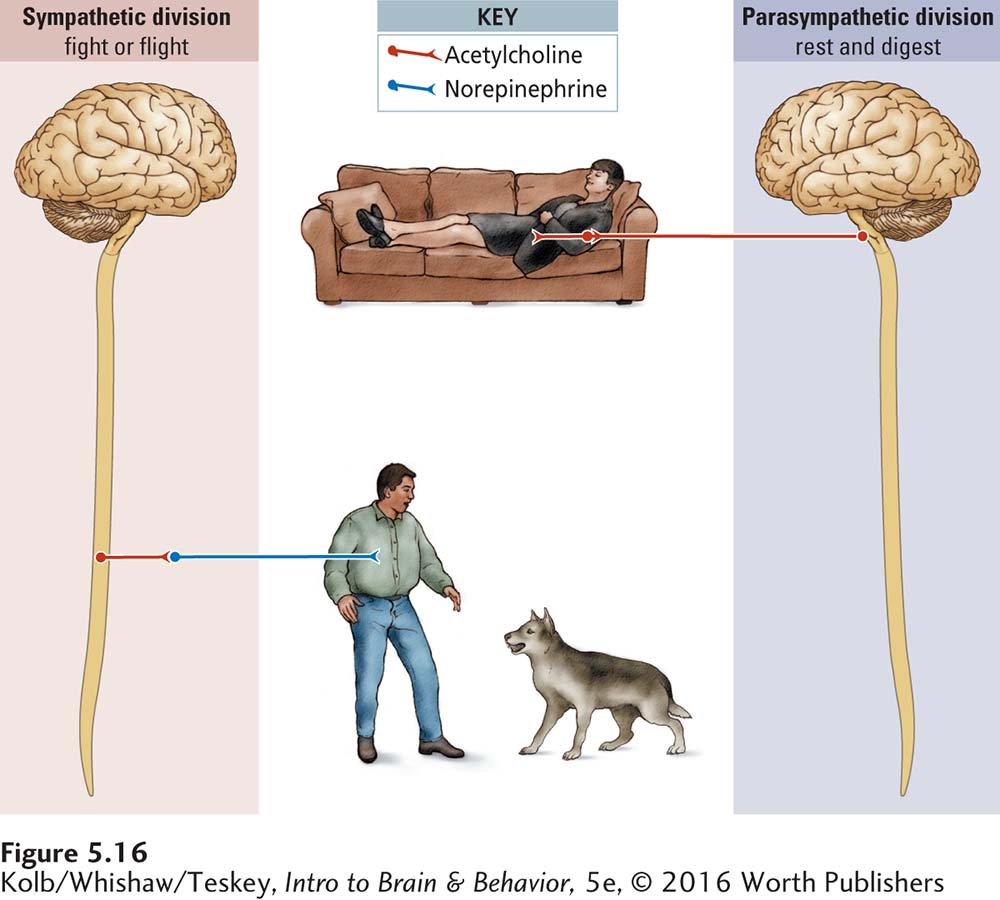
Which type of synapse is excitatory and which inhibitory depends on the particular body organ’s receptors. During sympathetic arousal, norepinephrine turns up heart rate and turns down digestive functions, because NE receptors on the heart are excitatory, whereas NE receptors on the gut are inhibitory. Similarly, acetylcholine turns down heart rate and turns up digestive functions because its receptors on these organs are reversed: on the heart, inhibitory; on the gut, excitatory. Neurotransmitter activity, excitatory in one location and inhibitory in another, mediates the sympathetic and parasympathetic divisions, forming a complementary autonomic regulating system that maintains the body’s internal environment under varying circumstances.
Enteric Nervous System Autonomy
The ENS can act without input from the CNS, which is why it has been called the second brain. It uses all four classes of neurotransmitters, more than 30 transmitters in total. Most are identical to those employed by the CNS. Chief among the small-
Sensory ENS neurons detect mechanical and chemical conditions in the system. Via intestinal muscles, motor neurons in the ENS control the mixing of intestinal contents. Secretion of digestive enzymes is also under ENS control.
Four Activating Systems in the Central Nervous System
Just as there is an organization to the neurochemical systems of the PNS, there is an organization of neurochemical systems in the CNS. These systems are remarkably similar across a wide range of animal species, which allowed for their identification, first in the rat brain and then in the human brain (Hamilton et al., 2010).
For each of the four activating systems that we describe here, a relatively small number of neurons grouped together in one or a few brainstem nuclei send axons to widespread CNS regions, suggesting that these nuclei and their terminals help to synchronize activity throughout the brain and spinal cord. You can envision an activating system as analogous to the power supply in a house. The fuse or breaker box is the source of the power, and from it transmission lines go to each room.
Just as in the ANS, the precise action of the CNS transmitter depends on the brain region that is innervated and on the types of receptors the transmitter acts on at that region. To continue our analogy, precisely what the activating effect of the power is in each room depends on the electrical devices in that room.
Each of four small-
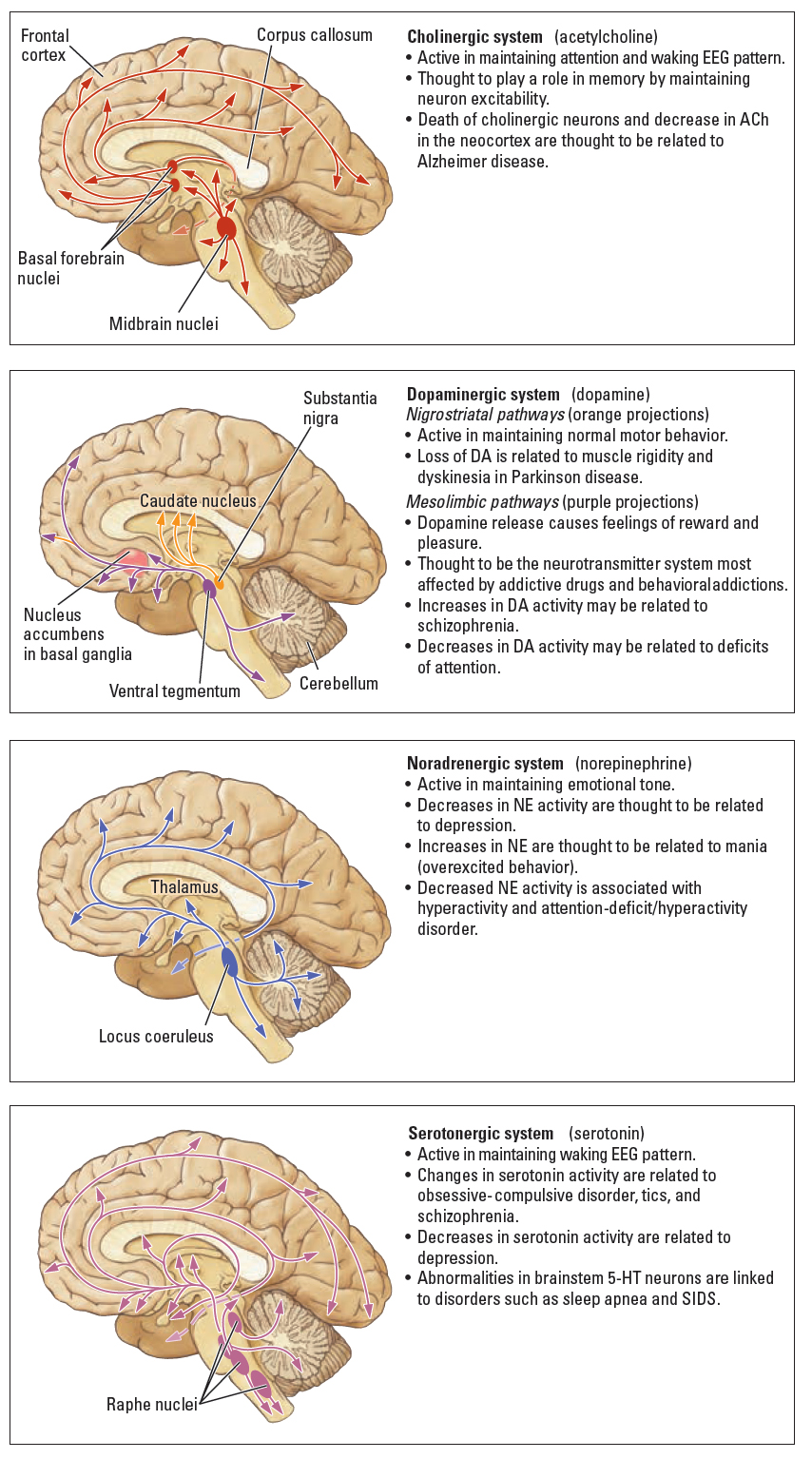
As summarized on the right in Figure 5-17, each CNS activating system is associated with numerous behaviors. Associations among activating systems, behavior, and brain disorders are far less certain. All these relations are subjects of ongoing research. Making definitive correlations between activating systems and behavior or activating systems and a disorder is difficult, because the axons of these systems connect to almost every part of the brain and spinal cord. They likely have both specific functions and modulatory roles. We detail some of the documented relations between the systems and behavior and disorders here and in many subsequent chapters.
Cholinergic System
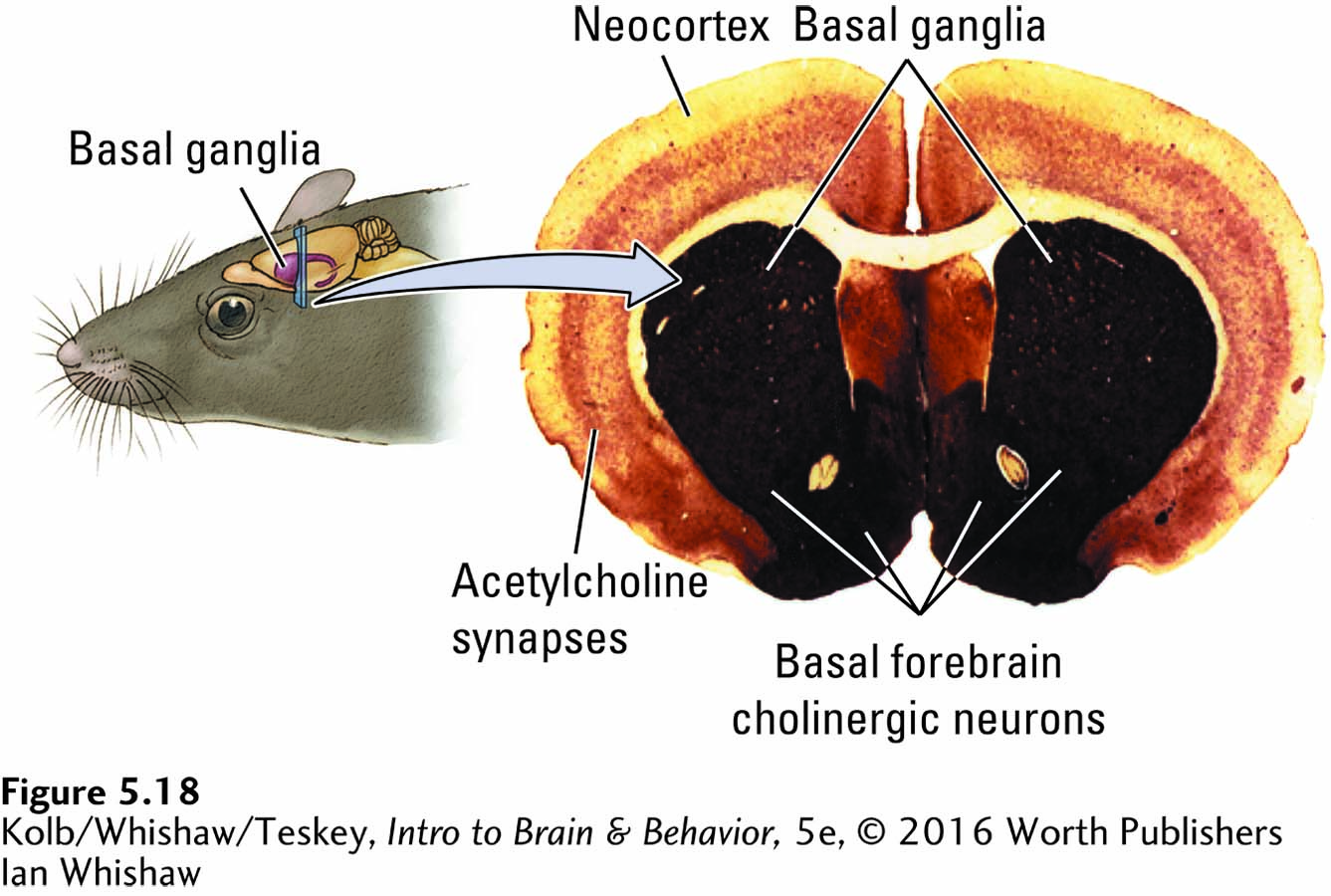
Figure 5-18 shows in cross section a rat brain stained for the enzyme acetylcholinesterase (AChE), which breaks down Ach in synapses, as diagrammed earlier in Figure 5-10. The darkly stained areas have high AChE concentrations, indicating the presence of cholinergic terminals. AChE permeates the cortex and is especially dense in the basal ganglia. Many of these cholinergic synapses are connections from ACh nuclei in the brainstem, as illustrated in the top panel of Figure 5-17.
The EEG detects electrical signals the brain emits during various conscious states; see Sections 7-2 and 13-3.
The cholinergic system participates in typical waking behavior, attention, and memory. For example, cholinergic neurons take part in producing one form of waking EEG activity. People affected by the degenerative Alzheimer disease, which begins with minor forgetfulness, progresses to major memory dysfunction, and later develops into generalized dementia, show a profound loss of cholinergic neurons at autopsy. One treatment strategy for Alzheimer disease is drugs that stimulate the cholinergic system to enhance alertness. But the beneficial effects of these drugs are minor at best (Herrmann et al., 2011). Recall that ACh is synthesized from nutrients in food; thus, the role of diet in maintaining acetylcholine levels also is being investigated.
Focus 14-3 details research on Alzheimer disease. Section 16-3 reviews dementias’ causes and treatments.
The brain abnormalities associated with Alzheimer disease are not limited to the cholinergic neurons, however. Autopsies reveal extensive damage to the neocortex and other brain regions. As a result, what role, if any, the cholinergic neurons play in the progress of the disorder is not yet clear. Perhaps their destruction causes degeneration in the cortex or perhaps the cause-
Dopaminergic System
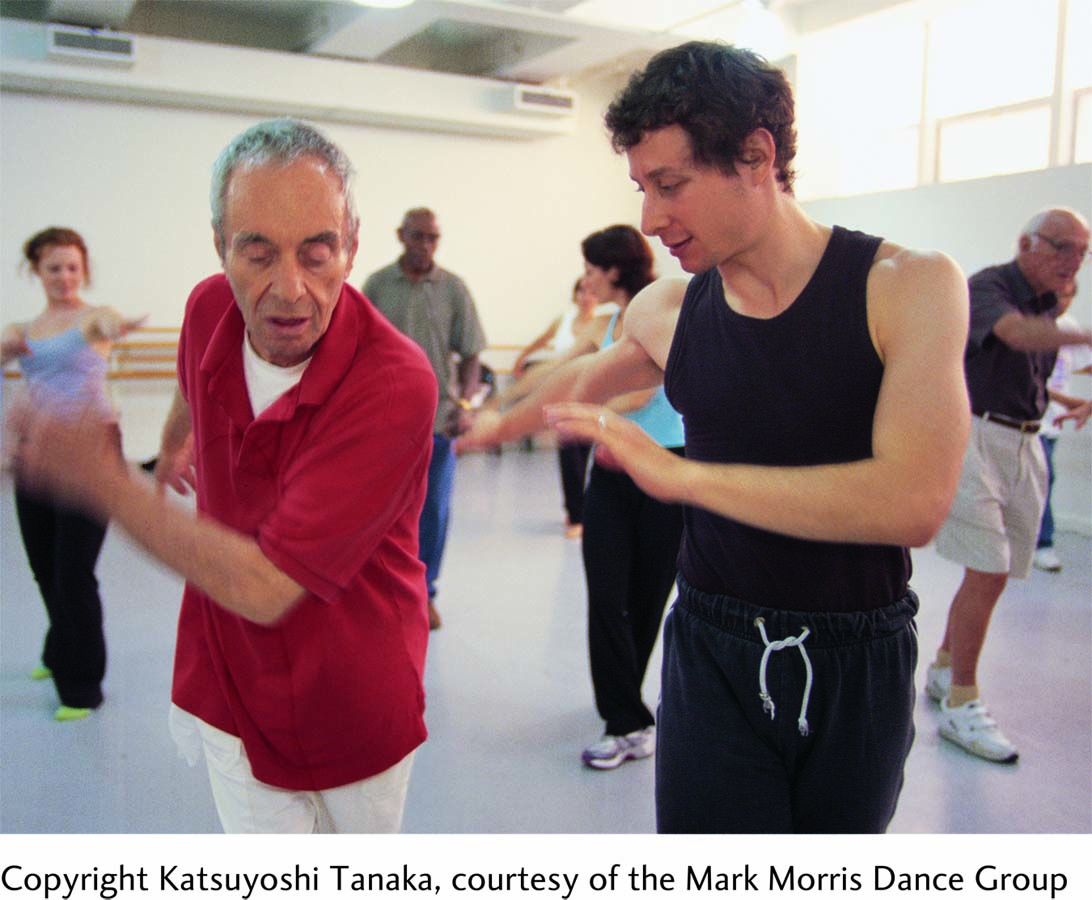
Figure 5-17 maps the dopaminergic activating system’s two distinct pathways. The nigrostriatal dopaminergic system plays a major role in coordinating movement. As described throughout this chapter in relation to parkinsonism, when dopamine neurons in the substantia nigra are lost, the result is a condition of extreme muscular rigidity. Opposing muscles contract at the same time, making it difficult for an affected person to move.
Parkinson patients also exhibit rhythmic tremors, especially of the limbs, which signals a release of formerly inhibited movement. Although the causes of Parkinson disease are not fully known, it can actually be triggered by the ingestion of certain toxic drugs, as described in Clinical Focus 5-4, The Case of the Frozen Addict. Those drugs may act as selective neurotoxins that specifically kill dopamine neurons in the substantia nigra.
Dopamine in the mesolimbic dopaminergic system may be the neurotransmitter most affected in addiction—
5-4
The Case of the Frozen Addict
Patient 1: During the first 4 days of July 1982, a 42-
Patient 1 was one of seven young adults hospitalized at about the same time in California. All showed symptoms of severe Parkinson disease that appeared very suddenly after drug injection. These symptoms are extremely unusual in this age group. All who were affected reportedly injected a synthetic heroin that was being sold on the streets in the summer of 1982.
J. William Langston (2008) and his colleagues found that the synthetic heroin contained a contaminant called MPTP (1-
The autopsy of one individual who was suspected of having died of MPTP poisoning showed that the brain had selectively lost dopamine neurons in the substantia nigra. The rest of the brain appeared healthy. Injecting MPTP into monkeys, rats, and mice produced similar symptoms and a similar selective loss of dopaminergic neurons in the substantia nigra. Thus, the combined clinical and experimental evidence indicates that a toxin can selectively kill dopamine neurons and that the die-
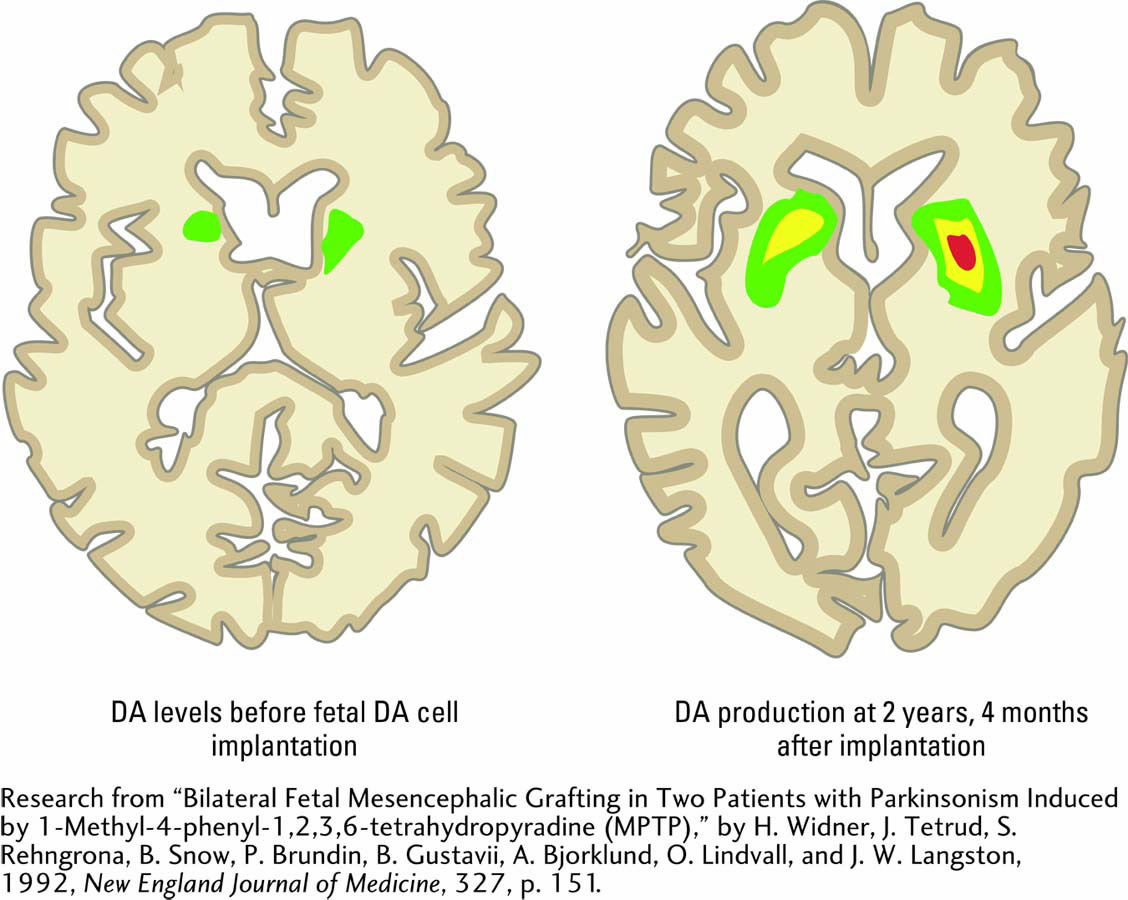
In 1988, Patient 1 received an experimental treatment at University Hospital in Lund, Sweden. Living dopamine neurons taken from human fetal brains at autopsy were implanted into the caudate nucleus and putamen (Widner et al., 1992). Extensive work with rodents and nonhuman primates in a number of laboratories had demonstrated that fetal neurons, before they develop dendrites and axons, can survive transplantation, mature, and secrete neurotransmitters.
Patient 1 had no serious postoperative complications and was much improved 24 months after the surgery. He could dress and feed himself, visit the bathroom with help, and make trips outside his home. He also responded much better to medication. The accompanying diagrams contrast DA levels in the brain of a Parkinson patient before (left) and 2 years, 4 months after implantation (right).
Transplantation of fetal neurons to treat Parkinson disease typically does not work. Unlike the case of the frozen addict, Parkinson disease is associated with a continuing, active process that destroys dopaminergic neurons, including transplanted neurons, in the substantia nigra. Because Parkinson disease can affect as many as 20 people per 100,000, scientists continue to experiment with new approaches to transplantation and with genetic approaches for modifying remaining dopamine neurons (Lane et al., 2010).
Sections 6-3, 6-4, and 12-3 describe drug effects on the mesolimbic DA system. Sections 6-2 and 7-4 discuss schizophrenia’s possible causes and Section 16-4, its neurobiology.
Excessive mesolimbic dopaminergic activity is proposed as well to play a role in schizophrenia, a behavioral disorder characterized by delusions, hallucinations, disorganized speech, blunted emotion, agitation or immobility, and a host of associated symptoms. Schizophrenia is one of the most common and most debilitating psychiatric disorders, affecting about 1 in 100 people.
Noradrenergic System
Norepinephrine (noradrenaline) may participate in learning by stimulating neurons to change their structure. Norepinephrine may also facilitate healthy brain development and contribute to organizing movements. A neuron that uses norepinephrine as its transmitter is termed a noradrenergic neuron (derived from adrenaline, the Latin name for epinephrine).
In the main, behaviors and disorders related to the noradrenergic system concern the emotions. Some symptoms of major depression—a mood disorder characterized by prolonged feelings of worthlessness and guilt, the disruption of typical eating habits, sleep disturbances, a general slowing of behavior, and frequent thoughts of suicide—
Serotonergic System
The serotonergic activating system maintains a waking EEG in the forebrain when we move and thus participates in wakefulness, as does the cholinergic system. Like norepinephrine, serotonin plays a role in learning, as described next in Section 5-4. Some symptoms of depression may be related to decreased activity in serotonin neurons, and drugs commonly used to treat depression act on 5-
Likewise, some research results suggest that various symptoms of schizophrenia also may be related to increases in serotonin activity, which implies that different forms of schizophrenia may exist. Decreased serotonergic activity is related to symptoms observed in obsessive-
5-3 REVIEW
Neurotransmitter Systems and Behavior
Before you continue, check your understanding.
Question 1
Although neurons can synthesize more than one _______, they are usually identified by the principal _______ in their axon terminals.
Question 2
In the peripheral nervous system, the neurotransmitter at somatic muscles is _______; in the autonomic nervous system, _______ neurons from the spinal cord connect with neurons for parasympathetic activity and with _______ neurons for sympathetic activity.
Question 3
The two principal small-
Question 4
The four main activating systems of the CNS are _______, _______, _______, and _______.
Question 5
How would you respond to the comment that a behavior is caused solely by a chemical imbalance in the brain?
Answers appear in the Self Test section of the book.