6-2 Grouping Psychoactive Drugs
Did you know that most psychoactive drugs and their effects were discovered by accident? Scientists and pharmaceutical companies have experimented ever since, to explain drug action, to synthesize alternative forms for therapeutic treatments, and to modify drugs to reduce side effects. But the process is complex. Drugs with similar chemical structure can have different effects, and drugs with different structure can have similar effects. And a single drug usually acts on many neurochemical systems and has many effects.
A full appreciation of any drug’s action requires a multifaceted description, such as can be found in compendiums of drug action. Unambiguously grouping psychoactive drugs is virtually impossible, because most drugs influence many behaviors. Behavioral descriptions undergo constant review, as illustrated by continuing revisions of the Diagnostic and Statistical Manual of Mental Disorders (DSM-
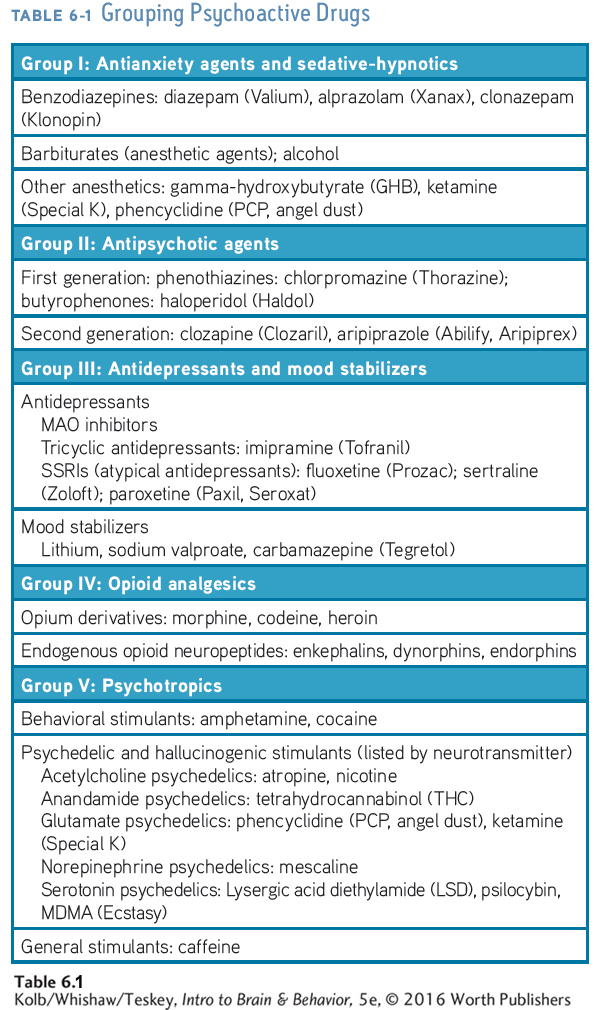
Table 6-1 groups psychoactive drugs based on their most pronounced behavioral or psychoactive effects (Advokat et al., 2014). Each of the five groups may contain a few to thousands of chemicals in its subcategories. In the following sections we highlight drug actions, both on neurochemical systems in the brain and on synaptic function.
Most psychoactive drugs have three names: chemical, generic, and branded. The chemical name describes a drug’s structure; the generic name is nonproprietary and is spelled lowercase; and the proprietary, or brand, name, given by the pharmaceutical company that sells it, is capitalized. Some psychoactive drugs also sport street names or are known as club drugs.
Group I: Antianxiety Agents and Sedative-Hypnotics
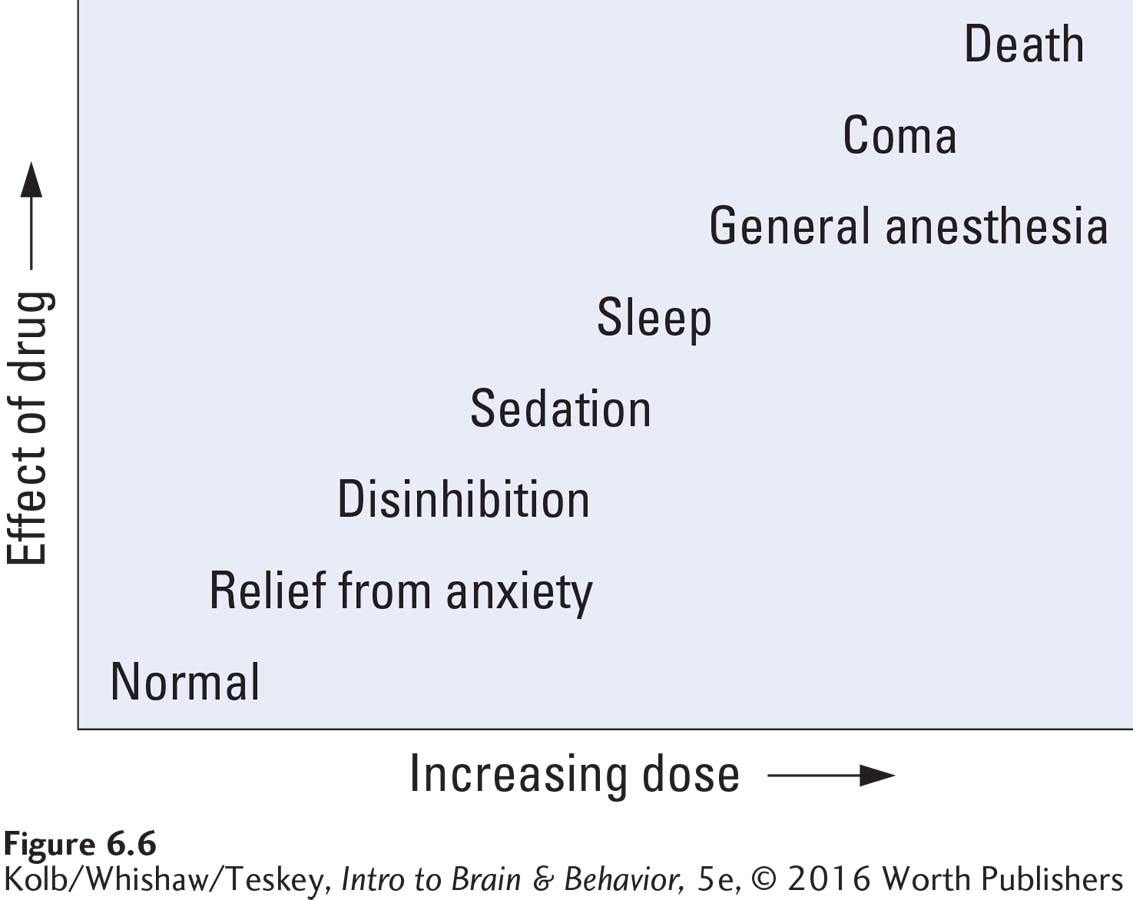
At low doses, antianxiety drugs and sedative-
Many psychoactive drugs have sedative-
Drug Action in the Brain
The best-
Sedative-
A characteristic feature of sedative-
Drug Action at the Synapse
GABA is an amino acid. Figure 5-12 shows its chemical structure.
Cross-
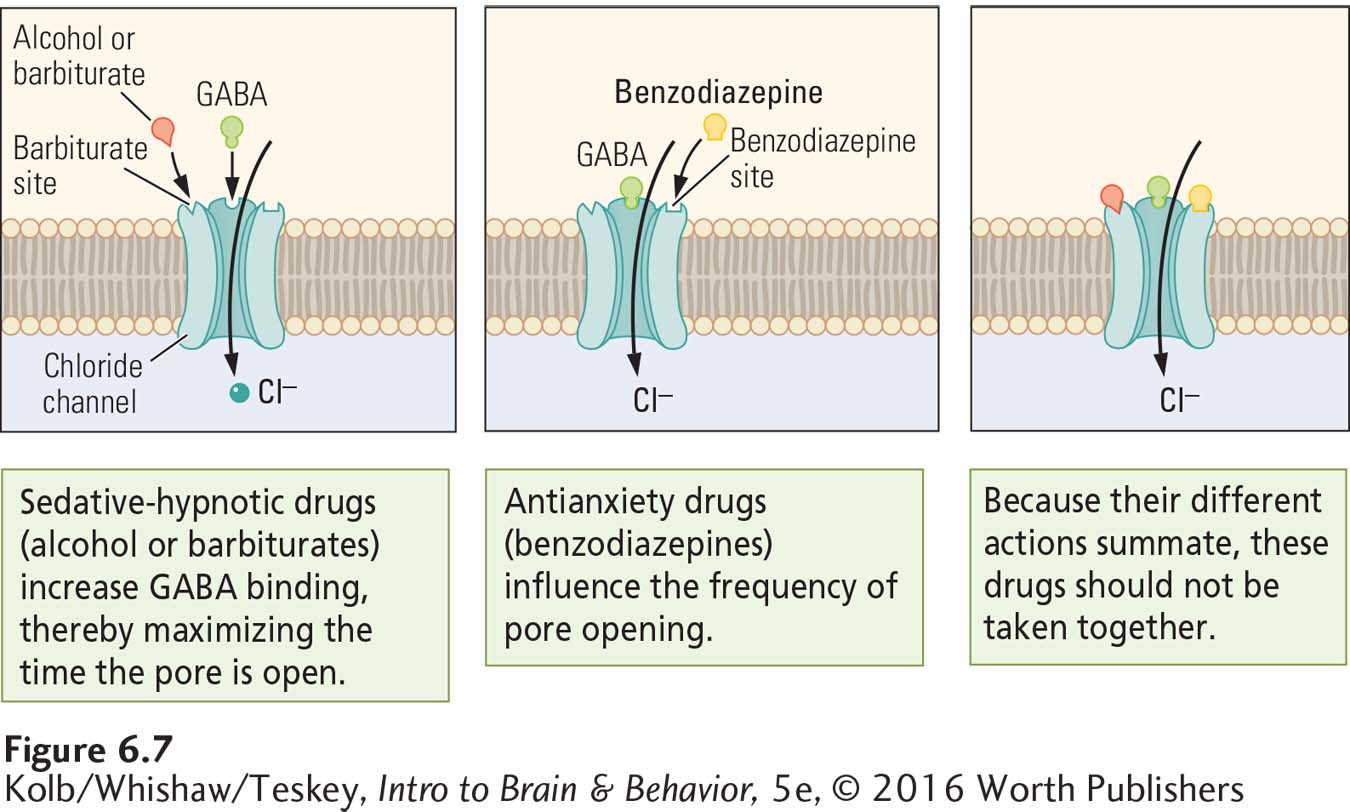
Excitation of the GABAA receptor produces an influx of Cl– through its pore. An influx of Cl– increases the concentration of negative charges inside the cell membrane, hyperpolarizing it and making it less likely to propagate an action potential. GABA therefore has its inhibitory effect by decreasing a neuron’s firing rate. Widespread reduction of neuronal firing underlies the behavioral effects of drugs that affect the GABAA synapse.
The GABAA receptor illustrated in Figure 6-7 has different binding sites for GABA, barbiturates, and benzodiazepines. Activation of each site promotes an influx of Cl–, but in different ways. Because the effects of actions at these three sites summate, sedative-
The GABAA receptor also has binding sites that block the ion pore when active, reducing the flow of Cl– and increasing the target neuron’s excitability. Picrotoxin, a compound that blocks the pore, produces epileptic discharges in postsynaptic neurons. Administering GABAA agonists can block picrotoxin’s action. Sedative-
Drugs that act on GABA receptors may affect brain development, because GABA is one of the substances that regulate brain development. Clinical Focus 6-2, Fetal Alcohol Spectrum Disorder, explores alcohol’s potentially devastating effects on developing fetuses.
6-2
Fetal Alcohol Spectrum Disorder
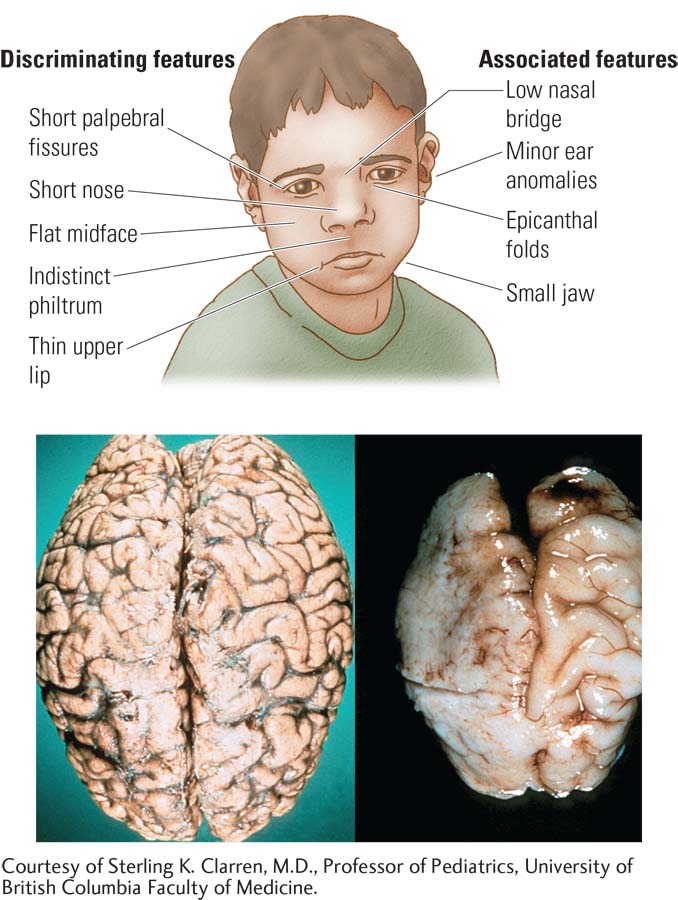
The term fetal alcohol syndrome (FAS) was coined in 1973 to describe a pattern of physical malformation and intellectual disability observed in some children born to alcoholic mothers. It is now called fetal alcohol spectrum disorder (FASD) to acknowledge the range of its effects. Children with FASD may have abnormal facial features, such as unusually wide spacing between the eyes. Their brains display a range of abnormalities, from small size with abnormal gyri to abnormal clusters of cells and misaligned cells in the cortex.
Related to these brain abnormalities are certain behavioral symptoms that children with FASD tend to have in common. They display varying degrees of learning disabilities and low intelligence test scores as well as hyperactivity and other social problems. Individuals with FASD are 19 times as likely to be incarcerated as those without it (Popova et al., 2011).
The offspring of approximately 6 percent of alcoholic mothers have pronounced FASD. In major cities, its incidence is about 1 in 700 births and is especially high among Native Americans on reservations in Canada, some other minority groups, and single mothers (Mead & Sarkar, 2014).
A major problem is that women who are most at risk for bearing FASD babies are poor and not well educated, their alcohol consumption problems predate pregnancy, and they have little access to prenatal care. It is often difficult to inform these women about the dangers that alcohol poses to a fetus and to encourage them to abstain from drinking before and while they are pregnant.
Alcohol-
Severe FASD is also more likely to coincide with binge drinking, which produces high blood alcohol levels. Other factors related to a severe outcome are poor nutritional health of the mother and the mother’s use of other drugs, including nicotine. In addition, alcohol use by mothers and fathers before conception can change the methylation status of some genes that contribute to disabilities found on the spectrum (Lee et al., 2015).
A major question raised by FASD is how much alcohol is too much to drink during pregnancy. To be completely safe, it is best not to drink at all in the months preceding as well as during pregnancy. This conclusion is supported by findings that as little as a single drink of alcohol per day during pregnancy can lead to a decrease in children’s intelligence test scores.
Group II: Antipsychotic Agents
The term psychosis is applied to behavioral disorders such as schizophrenia, which is characterized by hallucinations (false sensory perceptions) and delusions (false beliefs), among a host of symptoms. The use of antipsychotic drugs has improved the functioning of schizophrenia patients. Since 1955, when psychoactive drugs were introduced into widespread therapeutic use, resident patient populations in state and municipal mental hospitals in the United States have decreased dramatically.
The success of antipsychotic agents is an important therapeutic achievement, because the incidence of schizophrenia is high—
Antipsychotic agents have been widely used since the mid-
Antipsychotic agents’ therapeutic actions are not understood fully, and these drugs can produce many unwanted side effects. Joint experimentation by patients and physicians with different drugs and doses is common (Pouget et al., 2014). The dopamine hypothesis of schizophrenia holds that some forms of the disease may be related to excessive dopamine activity—
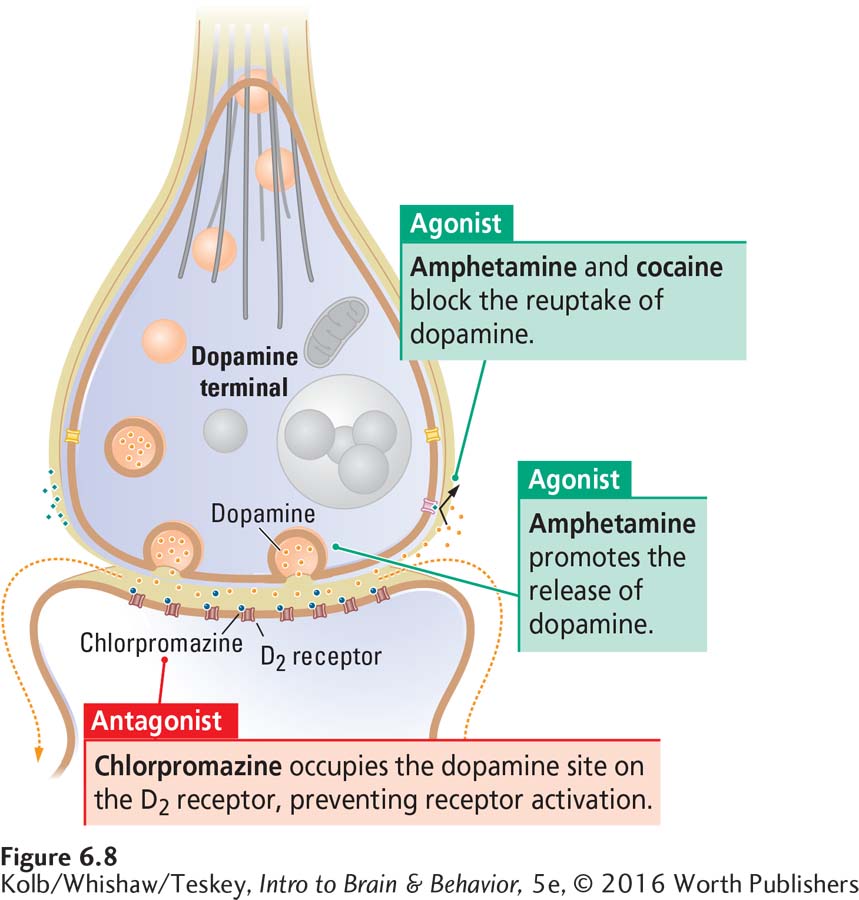
As Figure 6-8 shows, amphetamine is a dopamine agonist. It fosters dopamine release from the presynaptic membrane of D2 synapses and blocks dopamine reuptake from the synaptic cleft. The logic is that if amphetamine causes schizophrenialike symptoms by increasing dopamine activity, perhaps naturally occurring schizophrenia is related to excessive dopamine action too. Both FGAs and SGAs block the D2 receptor, which immediately reduces motor activity and alleviates the excessive agitation of some schizophrenia patients. Because schizophrenia involves more than just D2 receptors, changes in dopamine synapses do not completely explain the disorder or the effects of antipsychotic agents.
Group III: Antidepressants and Mood Stabilizers
Major depression—a mood disorder characterized by prolonged feelings of worthlessness and guilt, disruption of normal eating habits, sleep disturbances, a general slowing of behavior, and frequent thoughts of suicide—
Inadequate nutrition, stress from difficult life conditions, acute changes in neuronal function, and damage to brain neurons are among the factors implicated in depression. These factors may be related: nutritional deficiencies may increase vulnerability to stress; stress may change neuronal function; and if unrelieved, altered neuronal function may lead to neuron damage. Section 6-5 offers more information on stress.
Among the nutrient deficiencies that may be related to depression (Smith et al., 2010) are folic acid and other B vitamins and omega-
Section 12-4 explores the neuroanatomy of emotional disorders such as depression and Section 16-4 its neurobiology and treatments for it.
Not surprisingly, alongside improved nutrition, a number of pharmacological approaches to depression are available. They include normalizing stress hormones, modifying neuronal responses, and stimulating neuronal repair.
Antidepressant Medications
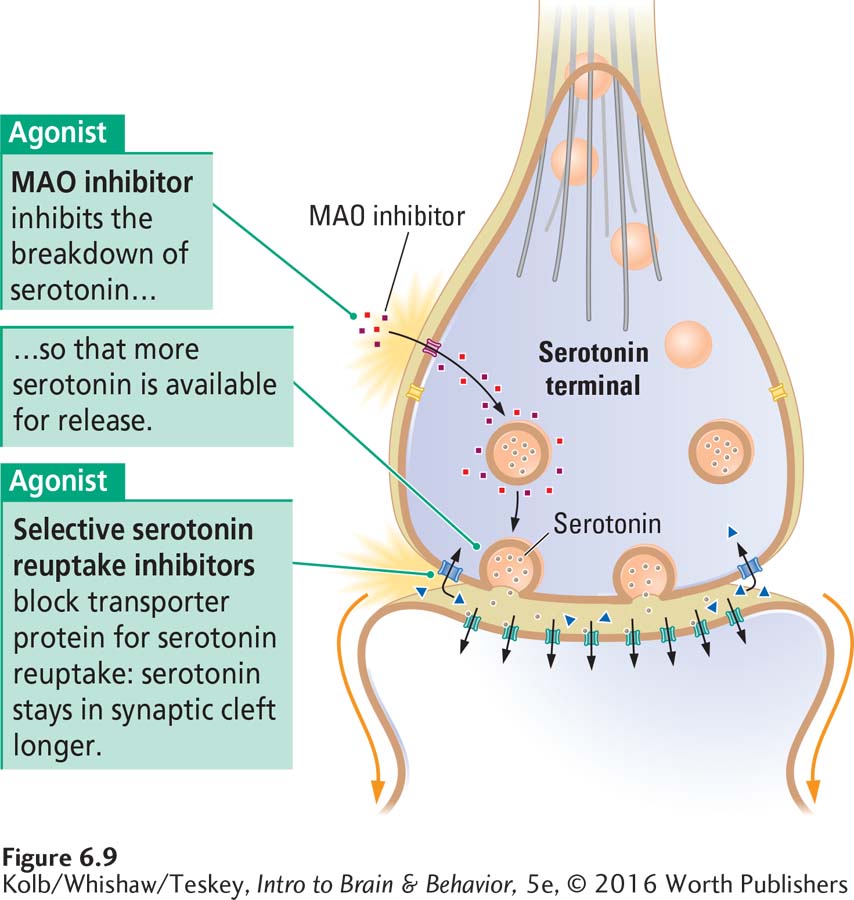
Three types of drugs have antidepressant effects: the monoamine oxidase (MAO) inhibitors; the tricyclic antidepressants, so called because of their three-
Antidepressants are thought to act by improving chemical neurotransmission at serotonin, noradrenaline (norepinephrine), histamine, and acetylcholine synapses, and perhaps at dopamine synapses as well. Figure 6-9 shows the actions of MAO inhibitors and second-
Reuptake is part of transmitter deactivation, the last of the four steps of neurotransmission (see Figure 5-4).
MAO inhibitors provide for more serotonin release with each action potential by inhibiting monoamine oxidase, an enzyme that breaks down serotonin in the axon terminal. In contrast, the tricyclics and second-
Although these drugs begin to affect synapses very quickly, their antidepressant actions take weeks to develop. One explanation is that antidepressants, especially SSRIs, stimulate second messengers in neurons to activate the repair of neurons damaged by stress. Of interest in this respect, one SSRI, fluoxetine (Prozac), increases the production of new neurons in the hippocampus, a limbic structure in the temporal lobes. As detailed in Section 6-5, the hippocampus is vulnerable to stress-
Most people recover from depression within a year of its onset. If left untreated, however, depression’s incidence of suicide is high, as described in Clinical Focus 6-3, Major Depression, on page 186. Of all psychological disorders, major depression is one of the most treatable, and cognitive and intrapersonal therapies are as effective as drug therapies (Comer, 2011).
Even so, about 20 percent of patients with depression fail to respond to antidepressant drugs. Accordingly, depression likely can have many other causes, including dysfunction in other transmitter systems and even brain damage, including frontal lobe damage. Some people have difficulty tolerating the side effects of antidepressants—
6-3
Major Depression
P. H. was a 53-
P. H. eventually consulted a physician, complaining of severe chest pains, which he feared signaled an impending heart attack. He informed his doctor that a heart attack would be a welcome relief because it would end his problems. The physician concluded that P. H. had depression and referred him to a psychiatrist.
Since the 1950s, depression has been treated with antidepressant drugs, a variety of cognitive-
The risk of suicide and self-
The glutamate antagonist ketamine, when given in smaller than anesthetic doses, can produce rapid beneficial effects that last for weeks, even in patients who are resistant to SSRI medication (Reinstatler and Youssef, 2015). Ketamine is thus proposed to be useful as an acute treatment for patients with major depression who are at risk for suicide and even for patients with bipolar depression who are at risk for suicide.
Prompted by complaints from family members that antidepressant drug treatments have caused suicide, especially in children, the U.S. Food and Drug Administration has advised physicians to monitor the side effects of SSRIs, including fluoxetine (Prozac), sertraline (Zoloft), and paroxetine (Paxil, Seroxat). Findings from several studies show no difference in the suicide rate between children and adolescents who receive SSRIs and a placebo, and the incidence of suicide after prescriptions were curtailed subsequent to the FDA warning actually increased (Isacsson and Rich, 2014).
Mood Stabilizers
Bipolar disorder, once referred to as manic-
The difficulty in treating bipolar disorder with drugs relates to the difficulty in understanding how a disease produces symptoms that appear to be opposites: mania and depression. Consequently, bipolar disorder often is treated with numerous drugs, each directed toward a different symptom. Mood stabilizers, which include the salt lithium, mute the intensity of one pole of the disorder, thus making the other less likely to occur. Lithium does not directly affect mood and so may act by stimulating mechanisms of neuronal repair, such as the production of neuron growth factors.
A variety of drugs for epilepsy (carbamazepine, valproate) have positive effects; perhaps they mute the excitability of neurons during the mania phase. And antipsychotic drugs that block D2 receptors effectively control the hallucinations and delusions associated with mania. It is important to remember, though, that all these treatments have side effects: enhancing beneficial effects while minimizing side effects is a major focus of new drug development (Grande and Vieta, 2015).
Group IV: Opioid Analgesics
An opioid is any compound that binds to a group of morphine-
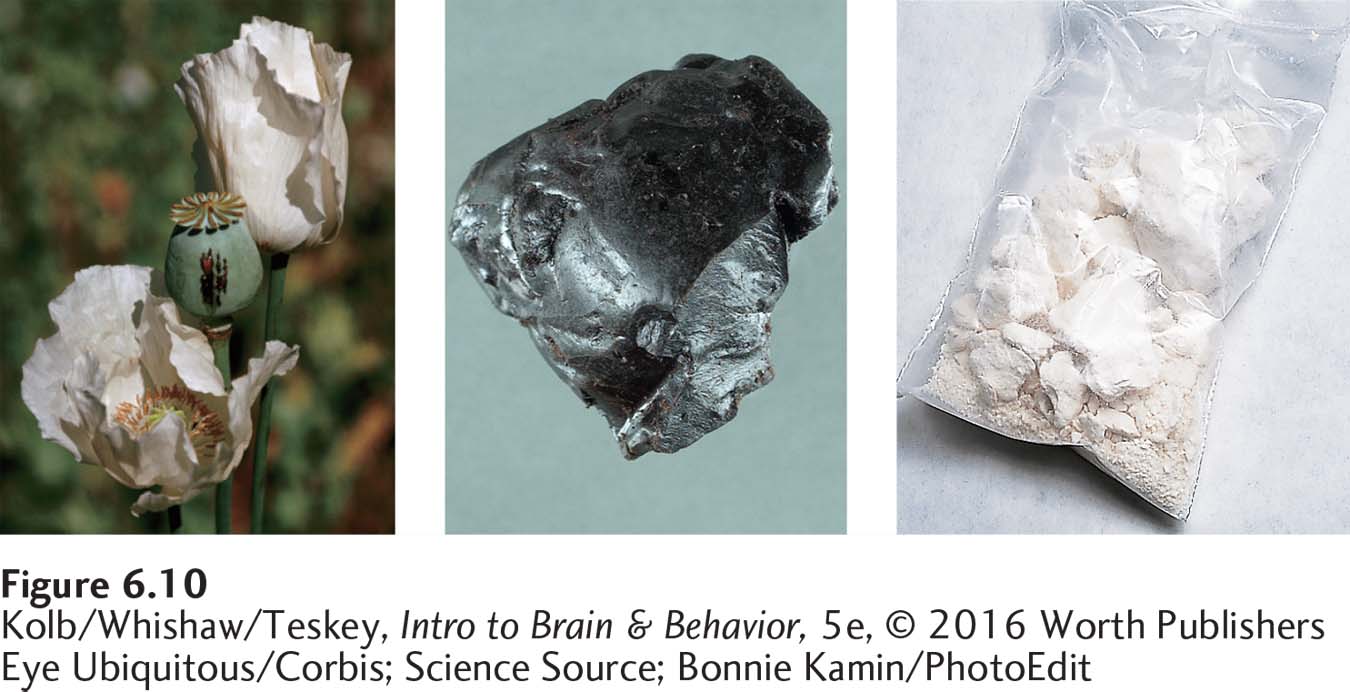
One source is opium, an extract of the seeds of the opium poppy, Papaver somniferum, shown at left in Figure 6-10 and named for Morpheus, the Greek god of dreams, is a powerful pain reliever. Despite decades of research, no other drug has been found that exceeds morphine’s effectiveness as an analgesic.
Eye Ubiquitous/Corbis
Science Source
Peptides, including the endorphins illustrated in Figure 5-13, are molecular amino acid chains connected by peptide bonds. Table 5-2 lists the families of peptide neurotransmitters.
The second natural source of opioids is the brain. In the 1970s, several groups of scientists injected radioactive opioids into the brain of experimental animals and identified receptors there to which opioids bind. At roughly the same time, other groups of investigators identified several brain peptides as the neurotransmitters that naturally affect these receptors. The peptides in the body that have opioidlike effects are collectively called endorphins (endogenous morphines).
Research has identified four classes of opioid peptides: endorphins, enkephalins, dynorphins, and endomorphins. The three receptors on which each endorphin is relatively specific are, respectively, mu, kappa, and delta. All endorphins and their receptors occur in many CNS regions as well as in other areas of the body, including the enteric nervous system. Morphine most closely mimics the endomorphins and binds most selectively to the mu receptors.
In addition to the natural opioids, synthetic opioids such as heroin affect mu receptors. Heroin, shown at right in Figure 6-10, is synthesized from morphine. It is more fat-
Among the synthetic opioids prescribed for clinical use in pain management are hydromorphone, levorphanol, oxymorphone, methadone, meperidine, oxycodone, and fentanyl. All opioids are potently addictive, and abuse of prescription opioids is growing more common. Opioids are also illegally modified, manufactured, and distributed. People who use opioids for relief of chronic pain and take them when they are not in pain can become addicted; some obtain multiple prescriptions and sell them illicitly.
Many drugs, including nalorphine (Lethidrone, Nalline) and naloxone (Narcan, Nalone), act as antagonists at opioid receptors. These drugs are competitive inhibitors: they compete with opioids for neuronal receptors. Because they can enter the brain quickly, they rapidly block the actions of morphine and so are essential aids in treating morphine overdoses. Many people addicted to opioids carry a competitive inhibitor as a treatment for overdosing. Because they can also be long-
Feeling and treating pain are topics in Section 11-4. Focus 12-1 reports that emotional pain activates the same neural areas as physical pain.
Researchers have extensively studied whether opioid peptides produced in the brain can be used as drugs to relieve pain without morphine’s addictive effects. The answer so far is mixed, and one of the objectives of pain research, producing an analgesic that does not produce addiction, may be difficult to realize.
Opioid drugs, such as heroin, are addictive and are abused worldwide. The hypodermic needle was developed in 1853 and used in the American Civil War for the intravenous injection of morphine for pain treatment. This practice is said to have produced 400,000 cases of the “Soldier’s Disease,” morphine addiction. Morphine has many routes of administration, but intravenous injection is preferred because it produces a euphoria described as a rush. Morphine does not readily cross the blood–
If opioids are used repeatedly, they produce tolerance such that within a few weeks the effective dose may increase tenfold. Thereafter, many desired effects with respect to both pain and addiction no longer occur. An addicted person cannot simply stop using the drug: a severe sickness called withdrawal results if drug use is abruptly stopped.
Because morphine results in both tolerance and sensitization, the morphine user is always flirting with the possibility of overdosing. The unreliability of appropriate information on the purity of street forms of morphine contributes to the risk. A lack of sterile needles for injections also leaves the morphine user at risk for many other diseases, including AIDS (acquired immunodeficiency syndrome) and hepatitis.
Opioid ingestion produces wide-
Group V: Psychotropics
Psychotropic drugs are stimulants that mainly affect mental activity, motor activity, arousal, perception, and mood. Behavioral stimulants affect motor activity and mood. Psychedelic and hallucinogenic stimulants affect perception and produce hallucinations. General stimulants mainly affect mood.
Behavioral Stimulants
Behavioral stimulants increase motor behavior as well as elevating mood and alertness. Rapid administration of behavioral stimulants is most likely to be associated with addiction. As shown in Figure 6-1, the quicker a drug reaches its target—
Section 5-1 describes experiments Otto Loewi performed to identify epinephrine, or adrenaline. Section 7-7 details symptoms and outcomes of ADHD and the search for an animal model of the disease.
Amphetamine is a synthetic compound. It was discovered in attempts to synthesize the CNS neurotransmitter epinephrine, which also acts as a hormone to mobilize the body for fight or flight in times of stress (see Figure 6-20). Both amphetamine and cocaine are dopamine agonists that act first by blocking the dopamine reuptake transporter. Interfering with the reuptake mechanism leaves more dopamine available in the synaptic cleft. Amphetamine also stimulates dopamine release from presynaptic membranes. Both mechanisms increase the amount of dopamine available in synapses to stimulate dopamine receptors. As noted in Focus 6-1, amphetamine-
One form of amphetamine was first used as an asthma treatment: Benzedrine was sold in inhalers as a nonprescription drug through the 1940s. Soon people discovered that they could open the container and ingest its contents to obtain an energizing effect. Amphetamine was widely used in World War II—
An illegal amphetamine derivative, methamphetamine (also known as meth, speed, crank, smoke, or crystal ice) continues in widespread use. Lifetime prevalence of methamphetamine use in the U.S. population, once estimated to be as high as 8 percent (Durell et al., 2008), is related to its ease of manufacture in illicit laboratories and to its potency, thus making it a relatively inexpensive, yet potentially devastating, drug.
Cocaine is a powder extracted from the Peruvian coca shrub, both shown in Figure 6-11. The indigenous people of Peru have chewed coca leaves through the generations to increase their stamina in the harsh environment and high elevations where they live. Refined cocaine powder can either be sniffed (snorted) or injected. Cocaine users who do not like to inject cocaine intravenously or cannot afford it in powdered form sniff or smoke rocks, or crack, a potent, highly concentrated form shown at right in Figure 6-11. Crack is chemically altered so that it vaporizes at low temperatures, and the vapors are inhaled.
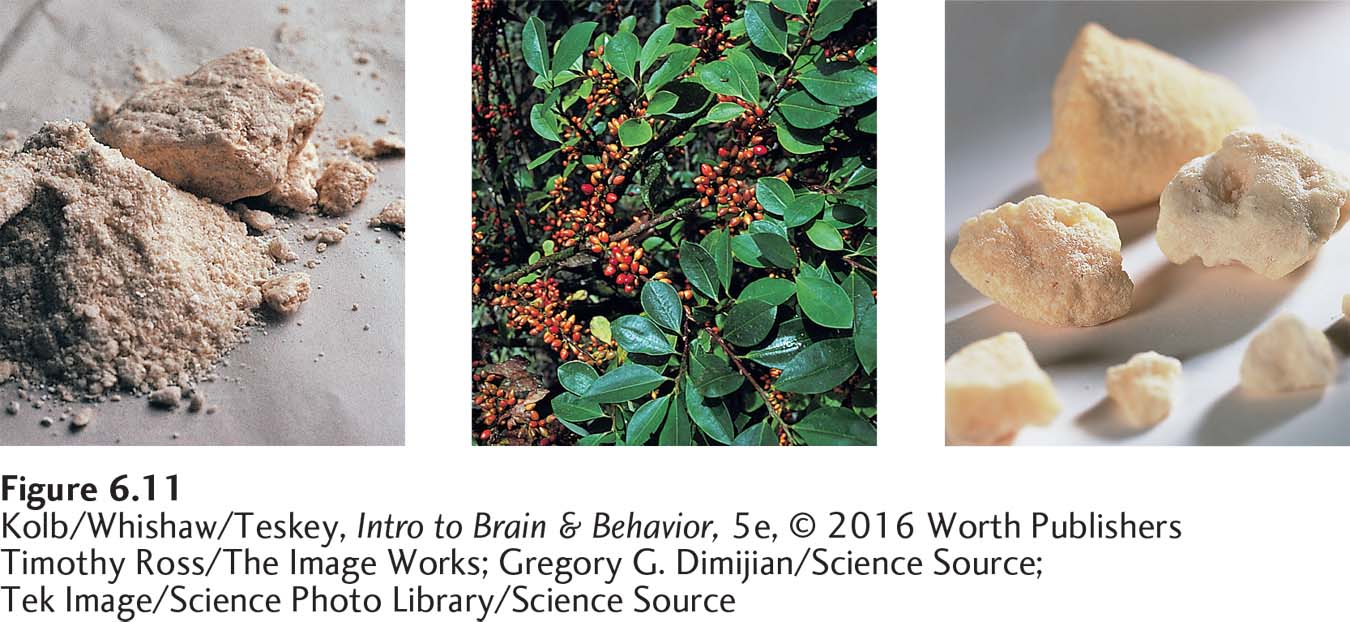
Gregory G. Dimijian/Science Source
Timothy Ross/The Image Works
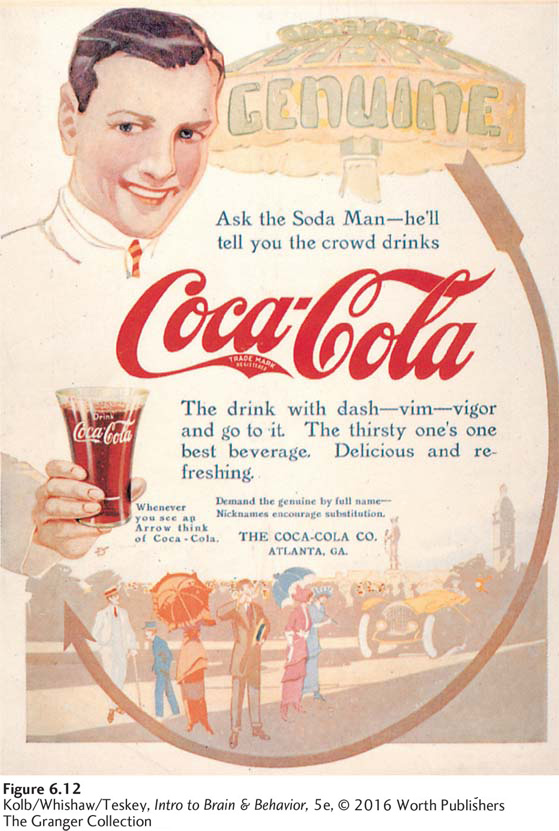
Sigmund Freud (1974) popularized cocaine in the late 1800s as an antidepressant. It was once widely used in soft drinks and wine mixtures promoted as invigorating tonics. It is the origin of the trade name of Coca-
Freud also recommended that cocaine be used as a local anesthetic. Cocaine did prove valuable for this purpose, and many derivatives, such as xylocaine (often called Novocain), are used today. These local anesthetic agents reduce a cell’s permeability to sodium ions and so reduce nerve conduction.
Psychedelic and Hallucinogenic Stimulants
Psychedelic drugs alter sensory perception and cognitive processes and can produce hallucinations. We categorize the major groups of psychedelics by their actions on specific neurotransmitters, here and in Table 6-1 on page 181.
ACETYLCHOLINE PSYCHEDELICS These drugs either block (atropine) or facilitate (nicotine) transmission at ACh synapses.
Anandamide (from Sanskrit, meaning joy or bliss) acts on a receptor that naturally inhibits adenyl cyclase, part of a second messenger system active in sensitization (see Section 5-4).
ANANDAMIDE PSYCHEDELICS Results from numerous lines of research suggest that the endogenous neurotransmitter anandamide enhances forgetting. Anandamide prevents the brain’s memory systems from being overwhelmed by all the information to which we are exposed each day. Tetrahydrocannabinol (THC) is one of 84 cannabinoids and the main psychoactive constituent in marijuana, obtained from the hemp plant Cannabis sativa, shown in Figure 6-13. THC alters mood primarily by interacting with the anandamide CB1 receptor found on neurons, and it also binds with the anandamide CB2 receptors found on glial cells and in other body tissues. THC has low toxicity but may have a detrimental effect on memory as well as a positive effect on mental overload.
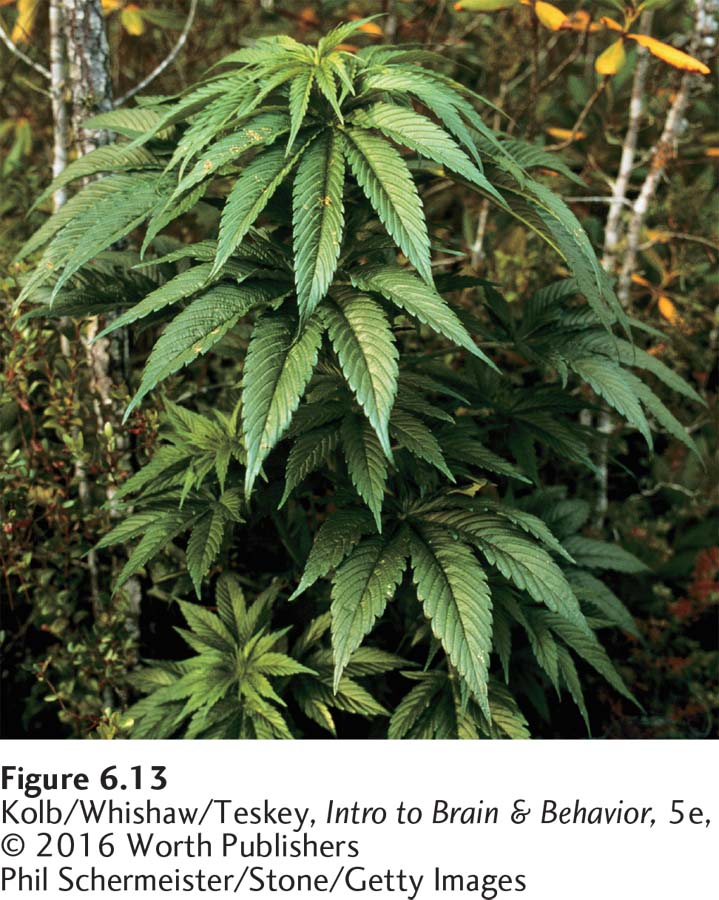
Evidence points to the usefulness of THC, or other cannabinoids, as a therapeutic agent for a number of disorders. It relieves nausea and emesis (vomiting) in patients undergoing cancer chemotherapy who are not helped by other treatments and stimulates the appetite in AIDS patients with anorexia–
Synthetic and derived forms of THC have been developed in part to circumvent legal restrictions on its use. Nevertheless, legal restrictions against THC use hamper investigations into its useful medicinal effects.
GLUTAMATE PSYCHEDELICS PCP (angel dust) and ketamine (Special K) can produce hallucinations and out-
Glutamate is the main excitatory neurotransmitter in the forebrain and cerebellum. Section 14-4 describes how Glu and NMDA receptors affect long-
Although PCP’s primary psychoactive effects last for a few hours, its total elimination rate from the body can extend its action for 8 days or longer. That psychotropic drugs, including PCP and ketamine, can produce schizophrenialike symptoms, including hallucinations and out-
NOREPINEPHRINE PSYCHEDELICS Mescaline, obtained from the peyote cactus, is legal in the United States for use by Native Americans for religious practices. Mescaline produces pronounced psychic alterations, including a sense of spatial boundlessness and visual hallucinations. The effects of a single dose last up to 10 hours.
SEROTONIN PSYCHEDELICS The synthetic drug lysergic acid diethylamide (LSD) and naturally occurring psilocybin (obtained from various mushrooms) stimulate some 5-
Serotonin psychedelics may stimulate other transmitter systems, including norepinephrine receptors. MDMA (Ecstasy), one of several synthetic amphetamine derivatives, induces a sense of well-
General Stimulants
General stimulants cause an overall increase in cells’ metabolic activity. Caffeine, a widely used stimulant, inhibits an enzyme that ordinarily breaks down the second messenger cyclic adenosine monophosphate (cAMP). The resulting increase in cAMP leads to increased glucose production, making more energy available and allowing higher rates of cellular activity.
Caffeine boosts cAMP concentrations, action potentials last longer than usual, and we get the coffee jitters.
A cup of coffee contains about 100 mg of caffeine; many common soft drinks contain almost as much; and some energy drinks pack as much as 500 mg. You may be using more caffeine than you realize. Excessive levels can lead to the jitters. Regular caffeine users who quit may have headaches, irritability, and other withdrawal symptoms.
6-2 REVIEW
Grouping Psychoactive Drugs
Before you continue, check your understanding.
Question 1
Because of their diverse actions, it is useful to group drugs in terms of their most pronounced ______ or ______ effects.
Question 2
Antianxiety and sedative-
Question 3
Among the antidepressant drug types, ______ increase the amount of 5-
Question 4
Opioids mimic the action of ______ by binding to the same receptors.
Question 5
Amphetamine stimulates ______ and cocaine blocks ______ at the ______ synapse.
Question 6
On which neurotransmitters do drugs that produce psychotropic effects act?
Answers appear in the Self Test section of the book.