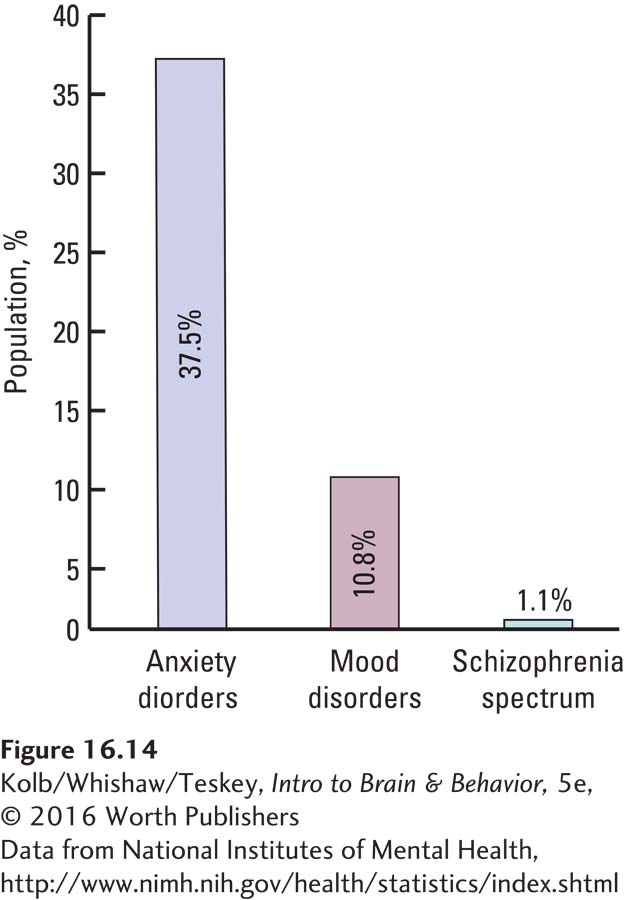
16-4 Understanding and Treating Psychiatric Disorders
The DSM-
Schizophrenia Spectrum and Other Psychotic Disorders
Psychoses are psychological disorders in which a person loses contact with reality, subject to irrational ideas and distorted perceptions. Among the varieties of psychosis, schizophrenia is the most common and best understood. Although it takes many forms, whether schizophrenia is a single disorder or several disorders that share some symptoms is uncertain. The complexity of behavioral and neurobiological factors that characterize schizophrenia makes it especially difficult to diagnose and classify. Understanding schizophrenia is an evolving process and far from complete.
Diagnosing Schizophrenia
The DSM lists six diagnostic symptoms of schizophrenia:
Delusions—
beliefs that distort reality Hallucinations—
distorted perceptions, such as hearing voices Disorganized speech, such as incoherent statements or senselessly rhyming talk
Disorganized behavior or excessive agitation
The opposite extreme of agitation: catatonic behavior
Negative symptoms, such as blunted emotions or loss of interest and drive, all characterized by the absence of some healthy response
The DSM criteria are subjective and more helpful in clinical diagnoses than in relating schizophrenia to objective, measurable brain abnormalities.
Neurobiology of Schizophrenia
Although schizophrenia may produce a wide range of symptoms, individual differences in behavioral effects exist as well. Voluminous research related to the origins and causes of schizophrenia has emerged, but the three lines of research summarized in this section have transformed ideas about its genetics, its development, and its associated brain correlates.
GENETICS It has long been recognized that genetics figures in schizophrenia, as does environment. The more closely related an individual is to someone diagnosed with schizophrenia, the more likely he or she is to develop the condition. The concordance of schizophrenia in identical twins is high: 50 percent is often cited. That the concordance for schizophrenia is not 100 percent means that environmental factors also play a role (Shorter & Miller, 2015).
It is also likely that many genes are associated with schizophrenia. Mutations on a number of chromosomes (candidates are 1, 6, 8, 13, and 22) predispose an individual to schizophrenia. It is also likely that many mutations in candidate genes on those chromosomes are involved. Genetic studies suggest that schizophrenia is probably a family of disorders and that the family may include other conditions, such as major depression and bipolar disorder (Claes et al., 2012). What may be common to the genes involved is that they contribute to brain development and so may contribute to various abnormalities in brain development.
DEVELOPMENT Typically, schizophrenia is diagnosed in young adulthood, but a body of evidence suggests that it originates much earlier, even prenatally. Its expression in adulthood must therefore await the conclusion of a host of developmental processes that ultimately shape the adult human brain. That schizophrenia has developmental origins has many implications.
First, environmental factors acting through epigenetic mechanisms are likely to influence brain development such that a subset of at-
BRAIN CORRELATES Many studies show anatomical changes in the brain associated with schizophrenia, especially in the temporal and frontal lobes.
Suggesting cell loss in these areas, the schizophrenic brain generally has large ventricles and thinner cortex in the medial temporal regions and frontal cortex.
Some aspects of neuronal and fiber composition of the temporal lobes and the frontal lobes are changed, as indicated by changes in their density imaged by MRI (Kong et al., 2012).
Alterations in neuronal structure show abnormal dendritic fields in cells in the dorsal prefrontal regions; as shown in Figure 16-15, in the hippocampus (Cho et al., 2004); and in the entorhinal cortex (Arnold et al., 1997).
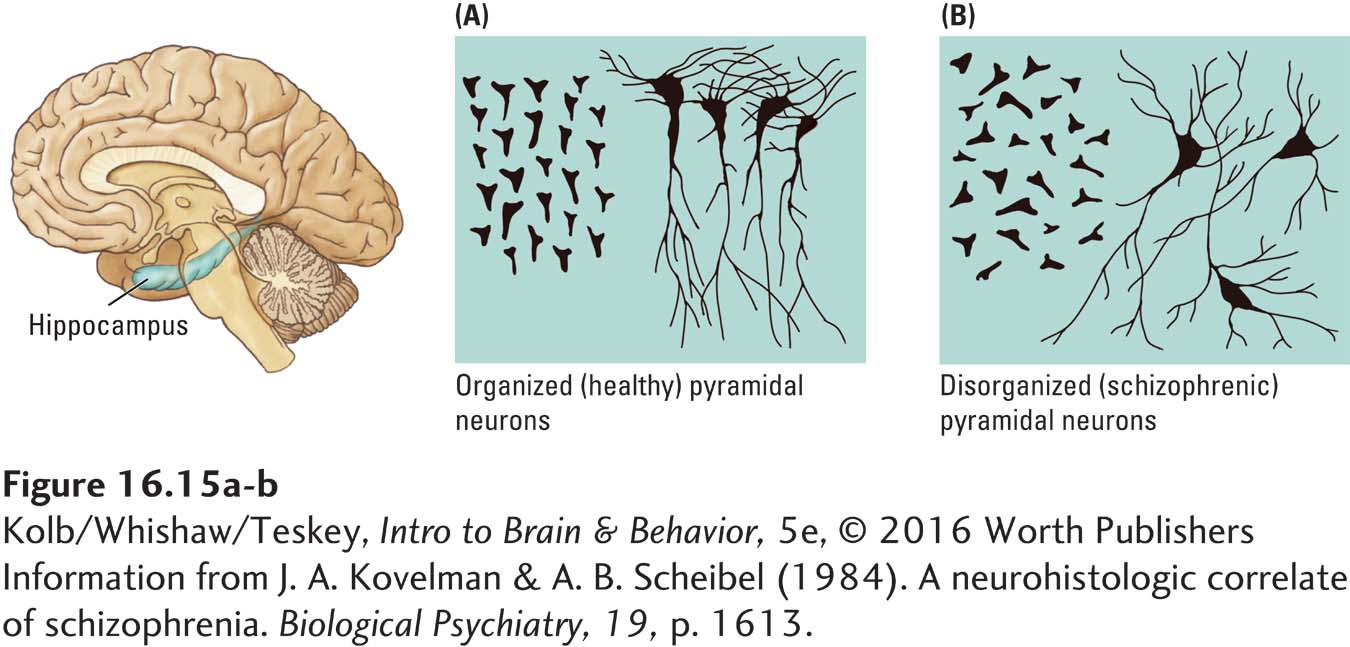
In sum, this evidence seems almost definitive in identifying schizophrenia as a developmental brain disorder associated in the main with alteration in the temporal and the frontal cortex. These brain regions are associated with memory, language, and decision making.
Neurochemical Correlates of Schizophrenia
Neuroleptics are antipsychotic drugs described in Section 6-2.
Neuroscientists also consider the neurochemical correlates of brain–
GABA is the brain’s main inhibitory neurotransmitter.
This dopamine theory of schizophrenia appears too simple, however, because many other neurochemical abnormalities, summarized in Table 16-6, are also associated with schizophrenia—
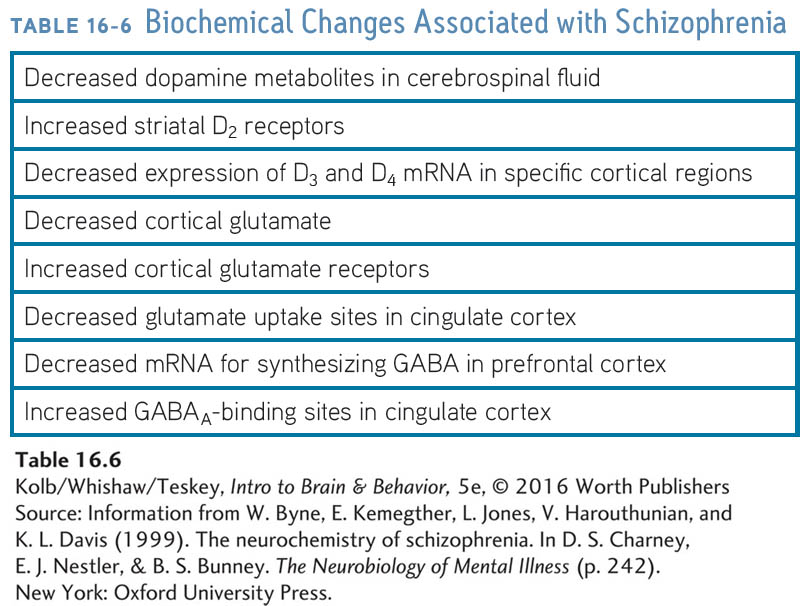
To summarize, schizophrenia is a complex disorder associated with abnormalities in brain structure and metabolism, especially in prefrontal and temporal cortex, and with neurochemical abnormalities in dopamine, glutamate, and GABA. Given the complexity of all these factors, it comes as no surprise that schizophrenia is so difficult to characterize and to treat.
Mood Disorders
Focus 6-3 explains the threat of suicide attendant to untreated major depression.
The DSM-
Mania, the opposite affective extreme from depression, is characterized by excessive euphoria, which the subject perceives as typical. The affected person often formulates grandiose plans and is uncontrollably hyperactive. Periods of mania often change, sometimes abruptly, to depression and back again to mania, a condition designated as bipolar disorder.
Neurobiology of Depression
Brain and environment both contribute to the complex neurobiology of depression. Predisposing factors related to brain anatomy and chemistry thus may contribute more to affective changes in some people, whereas life experiences contribute mainly to affective changes in other people. As a result, a bewildering number of life, health, and brain factors have been related to depression. These factors include economic or social failure, circadian rhythm disruption, vitamin D and other nutrient deficiency, pregnancy, brain injury, diabetes, cardiovascular events, and childhood abuse, among many others.
A major approach in neurobiological studies of depression is to ask whether a common brain substrate exists for depression. Antidepressant drugs acutely increase the synaptic levels of norepinephrine and serotonin, a finding that led to the idea that depression results from decreased availability of one or both neurotransmitters. Lowering their levels in healthy participants does not produce depression, however. And while antidepressant medications increase the level of norepinephrine and serotonin within days, it takes weeks for drugs to start relieving depression.
Section 14-4 explores the relation of hormones, trophic factors, and psychoactive drugs to neuroplasticity.
Among the various explanations suggested for these confounding results, none is completely satisfactory. Ronald Duman (2004) reviewed evidence to suggest that antidepressants act, at least in part, on signaling pathways, such as on cAMP, in the postsynaptic cell. Neurotrophic factors appear to affect antidepressant action and may underlie the neurobiology of depression. Investigators know, for example, that brain-
Given that BDNF acts to enhance the growth and survival of cortical neurons and synapses, BDNF dysfunction may adversely affect norepinephrine and serotonin systems through the loss of either neurons or synapses. Antidepressant medication may increase BDNF release through its actions on cAMP. Key here is that the cause of depression probably is not merely a simple decrease in transmitter levels. Many brain changes are related to depression.
Mood and Reactivity to Stress
Section 6-5 explains the neurobiology of the stress response—
A significant psychological factor in understanding depression is reactivity to stress. Monoamines—
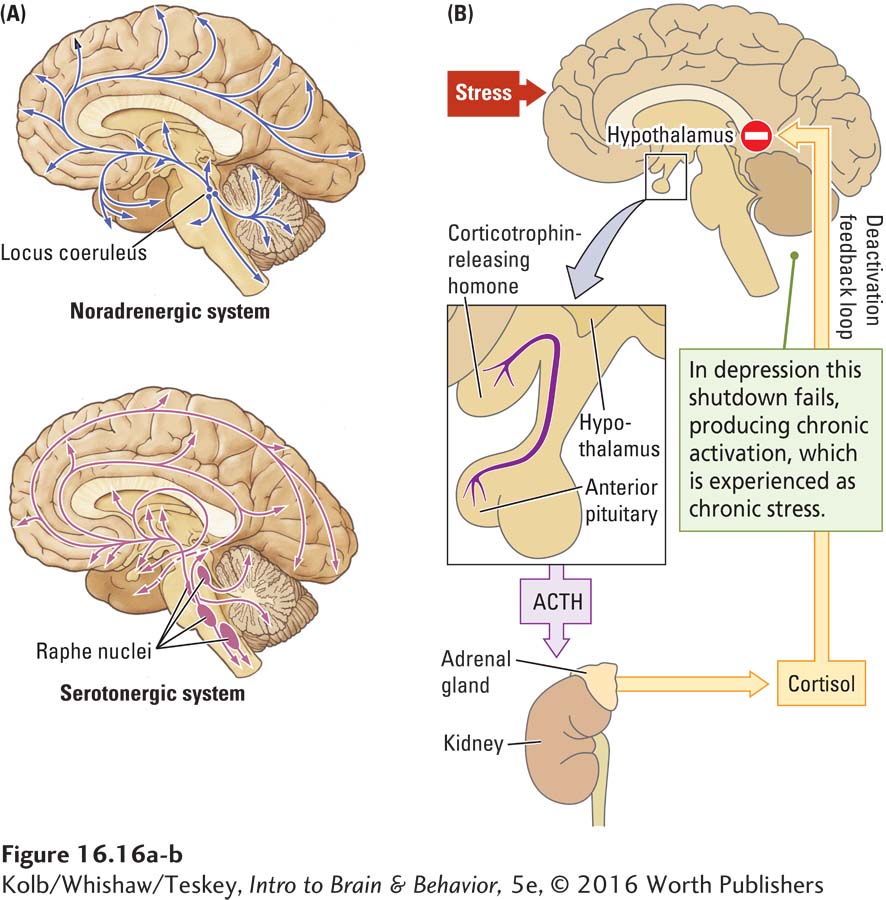
This research confirms studies on the effects of stress on hippocampal function reported in Sections 6-5, 7-5, and 8-4.
Excessive stress early in life may be especially detrimental. During critical periods in early childhood, abuse or other severe environmental stress can permanently disrupt HPA axis reactivity: it becomes constantly overactive. Overactivity in the HPA axis results in oversecretion of cortisol, an imbalance associated with depression in adulthood. Patrick McGowan and colleagues (2010) wondered if early experiences could alter gene expression related to cortisol activity in the HPA axis. They compared, postmortem, hippocampi obtained from suicide victims with a history of childhood abuse and hippocampi from other suicide victims with no childhood abuse or from controls. Abused suicide victims showed decreased gene expression for cortisol receptors relative to the controls. These results, derived from epigenetics, confirm that early neglect or abuse alters the HPA axis for life.
To summarize, the diffuse distribution of the norepinephrine-
Although we have emphasized biological correlates of depression, the best treatment need not be a direct biological intervention. Cognitive-
Simply pointing out that a person’s beliefs are faulty is not likely to be effective, however, because it probably took months or years to develop those beliefs. The neural circuits underlying faulty beliefs must change, just as the strategies for developing new ones must change. In a real sense then, CBT is effective if it induces neural plasticity and changes brain activity.
16-4
Antidepressant Action and Brain Repair
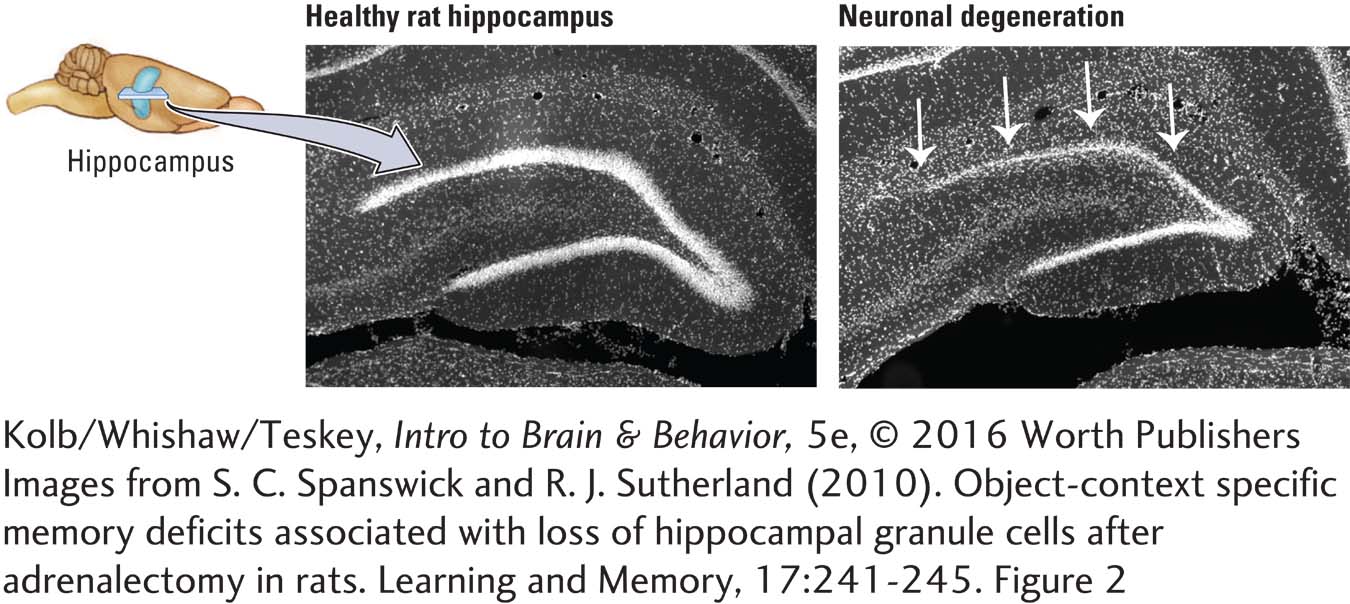
Excessive stress, poor coping skills, or both contribute to excessive cortisol levels in the brain and to depression and anxiety. Granule cells in the hippocampus, which are especially sensitive to cortisol, can die when cortisol levels either are reduced, as shown in the figure, or increased excessively.
These hippocampal cells may play a role in regulating cortisol levels and switching off the brain’s stress response. Their absence leaves the HPA axis unchecked. Then increased cortisol levels contribute to more neuron death and to depression and anxiety. It’s a vicious circle.
A remarkable finding emerged from studying how antidepressants such as fluoxetine (Prozac) and other selective serotonin reuptake inhibitors affect the hippocampus. The SSRIs increased neurogenesis in the subgranular zone, cell migration into the dentate gyrus, and the number of functioning cells there (Malberg et al., 2000).
That antidepressants take some weeks to produce their positive effects on behavior and that new neurons take some weeks to migrate and incorporate into the hippocampus suggest that the antidepressants’ mechanism of action is to enhance hippocampal function—
Luca Santarelli and colleagues (2003) used knockout mice that lacked a specific serotonin receptor (5-
Chronic antidepressant treatment affected only the mice with intact serotonin receptors, and only these mice displayed enhanced neurogenesis. Thus, because antidepressants activate serotonin receptors, serotonin must participate in enhancing neurogenesis.
The literature on hippocampal neurogenesis is the most prolific in neuroscience, represented by over 3000 papers reporting mainly on animal models. To summarize their findings, phenomena we perceive as bad (deprivation in infancy, conflict, stress, poor diet, most drugs) depress neurogenesis, and phenomena we perceive as good (exercise, enriched environment, sufficient sleep, good diet) enhance neurogenesis. Finding the signaling pathways that enhance neurogenesis may reveal the relationships among altered cognition, memory, depression, and the effects of antidepressant drugs (Costa et al., 2015).
Anxiety Disorders
Focus 12-3 describes symptoms of anxiety disorders; Section 6-5, how stress-
We are all subject to anxiety, usually acutely in response to stress or less commonly as chronic reactivity—
Imaging studies of people with anxiety disorders record increased baseline activity in the cingulate cortex and parahippocampal gyrus and enhanced responsiveness to anxiety-
Figure 12-18 diagrams these limbic system structures and charts their major connections.
Considerable interest has developed in investigating why some people show pathological anxiety to stimuli to which others have a milder response. One hypothesis, covered earlier, in the section on depression, is that stressful experiences early in life increase susceptibility to a variety of behavioral disorders, especially anxiety disorders.
Although anxiety disorders used to be treated primarily with benzodiazepines, such as Valium, now they are also treated with SSRIs, such as Prozac, Paxil, Celexa, and Zoloft. Antidepressant drugs do not act immediately, however, suggesting that the treatments must stimulate some gradual change in brain structure, much as these drugs act in treating depression.
One more time: a pill is not a skill.
Cognitive-
16-4 REVIEW
Understanding and Treating Behavioral Disorders
Before you continue, check your understanding.
Question 1
Schizophrenia is a complex disorder associated with neurochemical abnormalities in ____________, ____________, and ____________.
Question 2
Schizophrenia is associated with pronounced anatomical changes in the ____________ and ____________ cortices.
Question 3
The monoamine-
Question 4
The most effective treatment for depression and anxiety disorders is ____________.
Question 5
Describe the main difficulty in linking genes to schizophrenia.
Answers appear in the Self Test section of the book.