16-2 Classifying and Treating Brain and Behavioral Disorders
Figure 8-31 pegs the peak age of onset for mental disorders at 14 years.
Behavioral disorders afflict millions every year. The National Institute for Mental Disorders estimates that in a given year about one in four people in the United States has a diagnosable behavioral disorder, and nearly half of the population does over their lifetime. Only a minority receive treatment of any kind, and even fewer receive treatment from a mental health specialist. Large-
Identifying and Classifying Behavioral Disorders
Epidemiologists study disease distribution and causes in human populations and help define and assess behavioral disorders of three general types—
The first set of criteria for diagnoses in psychiatry was developed in 1972. Since that time, three parallel sets of criteria have gained prominence, and new versions appear periodically. One is the most recent edition of the World Health Organization’s International Classification of Diseases (ICD-
In addition, the Society for Clinical Psychology provides a list of psychological disorders, their symptoms, and a summary of psychological treatments. The National Institute of Neurological Disorders and Stroke provides a list of neurological disorders, including their symptoms, treatments, and any clinical trials that are investigating treatments. Classification systems organize knowledge about disorders and their treatments and are useful for decision making in such institutions as insurance companies, courts, and schools.
Section 12-5 explores the relationship among sexual orientation, sexual identity, and brain organization; and Section 15-5, sex differences in cognitive organization.
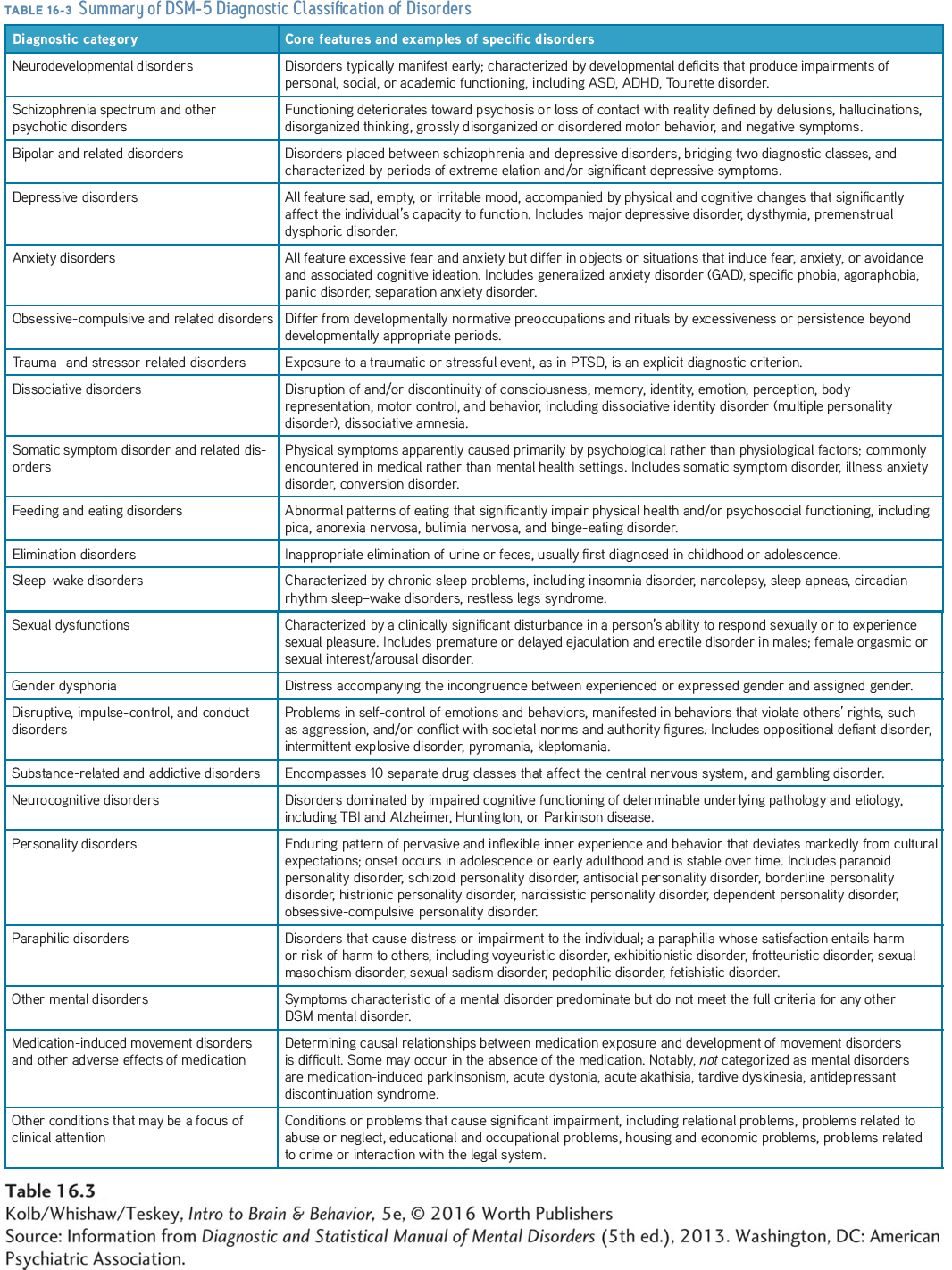
Table 16-3 summarizes the classification scheme used currently in the DSM-
Focus 8-2 describes the autism spectrum.
Each revision of any classification system reflects new perspectives. For example, the DSM-
Among the continually emerging means of searching for indicators of behavioral disorders, genetics and brain imaging, including MRI and PET, stand out. Although these tools are not currently used clinically, they are increasingly used both to classify disorders and to monitor treatment effectiveness. But to be useful, imaging test resolution, for example, must be sensitive enough to detect unique features of brain disorders and specific enough to rule out similar conditions. This sets a high bar, because many behavioral disorders display similar abnormalities. Enlarged ventricles, indicating a loss of brain cells, may appear in schizophrenia, Alzheimer disease, alcoholism, or head trauma, for example.
Nonetheless, imaging technology is shedding new light on behavioral disturbances. Imaging the brain structure, connections, and chemistry of subjects with childhood-
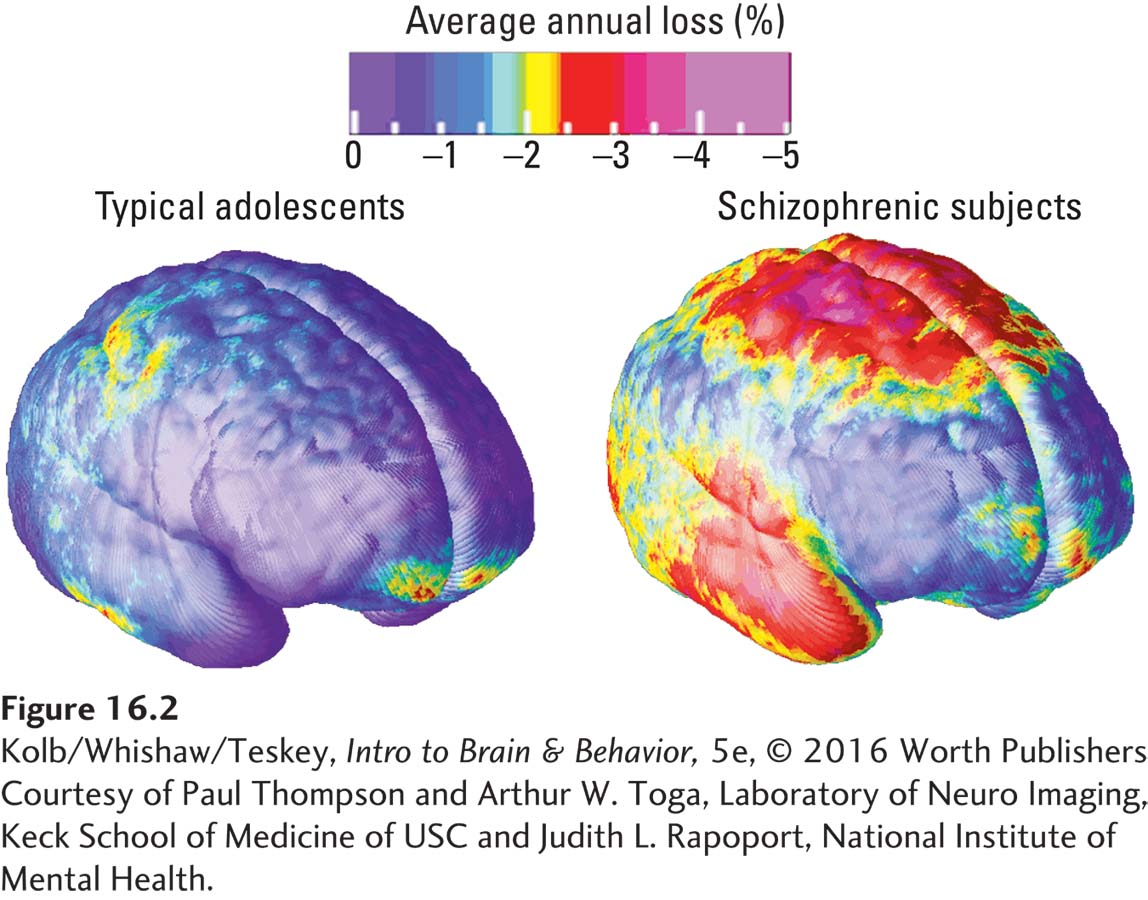
Abnormalities found throughout the brain vary by functional region and correlate with the onset of behavioral disturbances characteristic of schizophrenia. Not all disorders show such obvious loss of tissue but may show abnormal blood flow or metabolism that can be detected by either fMRI or PET. The PET images in Figure 16-3 illustrate metabolic changes in adult-
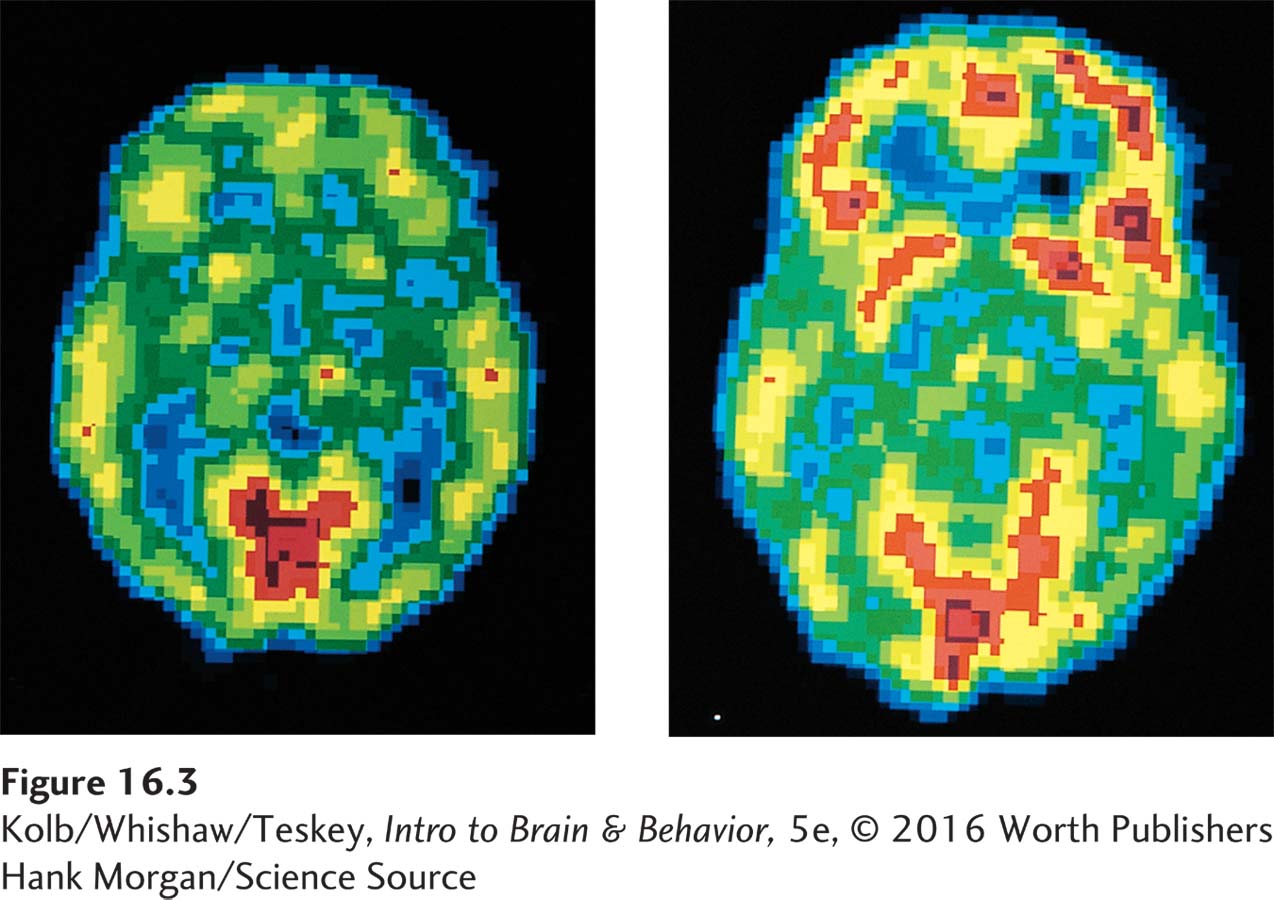
Combining behavioral diagnoses with genetic analysis and neuroimaging will move practitioners beyond symptom checklists to objective medical diagnoses. Imaging analyses will help target treatments to reduce the severity of such serious disorders as schizophrenia and Alzheimer disease. Current imaging techniques do not detect all brain pathology. It is not whether a gene is present or absent but whether that gene is or is not expressed that is relevant to its effects. The challenge lies in improving current techniques and in developing others that can identify subtler nervous system abnormalities.
The Basics in Section 1-3 overviews taxonomy.
Classification systems such as taxonomy, the branch of biology that groups organisms according to their common characteristics and relationships, have advanced our knowledge of brain structure and function. Likewise, classifications of behavioral disorders produced by the behavioral sciences have advanced understanding. Yet classification systems have their critics. One criticism is that “just because you name a disorder does not mean it exists.” Another is that changing societal views result in the inclusion or exclusion of disorders, as with sexual relationships other than heterosexuality.
Naming disorders becomes problematic as well. The term idiot once designated a person with a low IQ score. When the term became pejorative, it was replaced with the term retarded. That term then became pejorative, and the DSM-
Treatments for Disorders
The conditions listed in the Index of Disorders constitute a mere fraction of the total.
An inclusive list of brain and behavioral disorders would number in the thousands, including, on the organic side, genetic and developmental disorders, infectious diseases, nervous system injuries, and degenerative dementias. Behavioral disorders would include PTSD among the anxiety-
The ultimate goal for behavioral neuroscientists lies in applying their knowledge to generate treatments that can restore a disordered brain to a range of healthy functioning. This goal is daunting because the first task is so difficult: learning what causes a particular behavioral disturbance. Few behavioral disorders have a cause as simple as PKU does. Most, like schizophrenia, are complex. A more achievable goal is to make small advances by improving current treatments, to develop new treatments, and to analyze disease causes. Available treatments, while extensive, fall into four general categories:
Neurosurgical. The skull is opened and some intervention is performed on the brain.
Electrophysiological. Brain function is modified by stimulation through the skull.
Pharmacological. A chemical that affects the brain is either ingested or injected.
Behavioral. Treatment manipulates the body or the experience, which in turn influences the brain.
Neurosurgical Treatments
Neurosurgical manipulation of the nervous system is largely reparative, as when tumors are removed or arteriovenous (AV) malformations corrected. Typically, such neurosurgical interventions are successful. Advances include improved imaging of a target for surgery—
Treatment for Parkinson disease entails inactivating brain regions that produce tremors and regions participating in the production of muscular rigidity that impairs movement. An electrode is placed in the motor thalamus and an electric current used to damage neurons responsible for producing the unwanted effects. Alternatively, in deep brain stimulation (DBS), an electrode fixed in place in the globus pallidus or subthalamic nucleus is connected to an external electrical stimulator that the patient can activate (Figure 16-4). The stimulation can inactivate cells responsible for unwanted effects and so restore more normal movement (Knight et al., 2015).
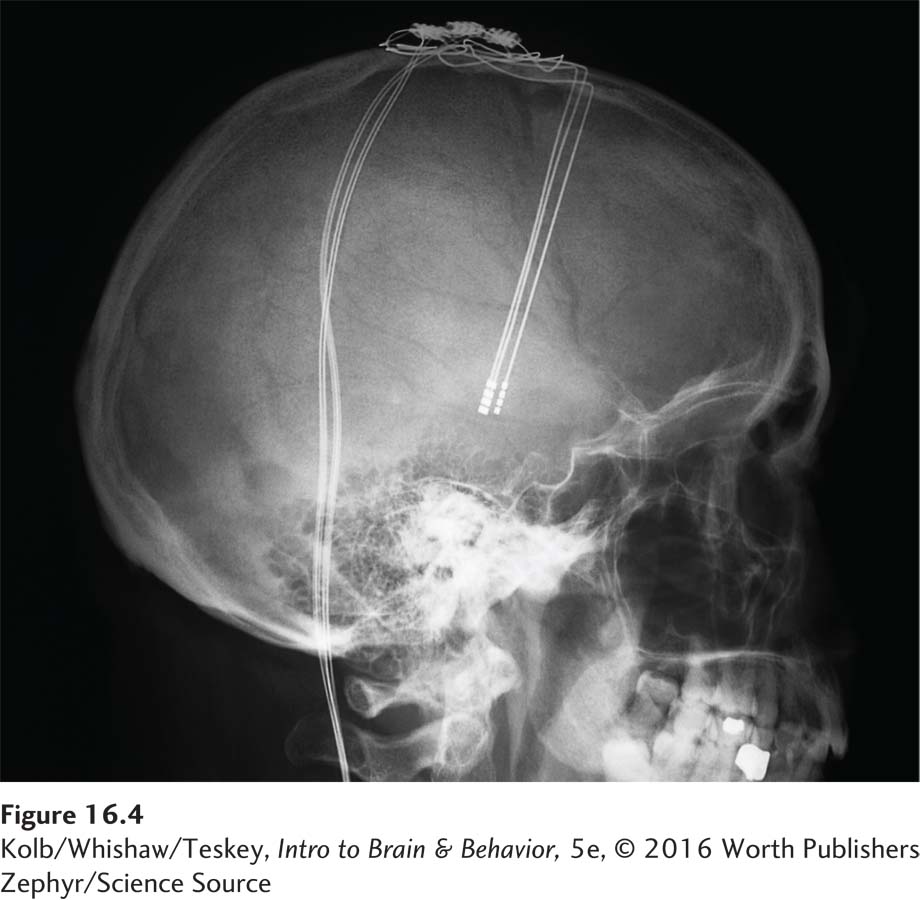
DBS is also used experimentally to treat traumatic brain injury (TBI) and behavioral dysfunctions such as obsessive-
Figure 14-26 shows neurogenesis induced in a rat brain to repair a cortical stroke.
Another highly experimental neurosurgical strategy draws on the fixed sequence of prenatal brain development from cell division and cell differentiation to cell migration and synaptogenesis. If a brain region is functioning abnormally or if it is diseased or dead, as occurs in TBI or after a stroke, it should be possible to return this region to the embryonic state and regrow a healthy region. The use of so-
In the 1980s, neurosurgeons experimented with implanting fetal stem cells in adult brains. Success was limited due to difficulties in cell placement and connections and rejection by the patient’s immune system. Another restorative idea comes from the discovery that multipotent stem cells in other body regions, such as bone marrow and skin, appear capable of manufacturing neural stem cells. Indeed, using appropriate manipulations, any cell can potentially be returned to a stem cell state. The advantage is that the patient’s own cells are not rejected by the immune system.
Figure 8-8 diagrams the origins of specialized brain cells from multipotent neural stem cells.
If people’s own multipotent stem cells prove practical for generating neural stem cells, it should be possible to extract stem cells, place them in a special culture medium to generate thousands or millions of cells, and place these stem cells in the damaged brain. The cells would be instructed to differentiate appropriately and develop the correct connections. Stem cell transplantation is taken seriously today as a potential treatment for disorders such as TBI and stroke, but it remains largely at an investigative stage (Savitz, 2015).
Electrophysiological Treatments
Treating the mind by treating the body is an ancient notion. In the 1930s, researchers used insulin to lower blood sugar and produce seizures as a treatment for depression. By the 1950s, insulin therapy had been replaced by electroconvulsive therapy (ECT), the first electrical brain stimulation treatment.
Neurotrophic factors, nourishing chemical compounds, support neuronal growth, development, and viability.
ECT was developed as a treatment for otherwise untreatable depression, and although its mode of action was not understood, it did prove useful. Although rarely used today, ECT sometimes remains the only treatment that works for people with severe depression. One reason may be that it stimulates the production of a variety of neurotrophic factors, especially BDNF (brain-
Figure 7-7 diagrams how TMS works.
Problems with ECT include the massive convulsions electrical stimulation causes. Large doses of medication are normally required to prevent them. ECT also leads to memory loss, a symptom that can be troublesome with repeated treatments. A noninvasive technique, transcranial magnetic stimulation (TMS), uses magnetic rather than electrical stimulation. Magnetic stimulation can be applied to a localized brain region. Anesthesia is not necessary. TMS is an FDA-
16-2
Treating Behavioral Disorders with Transcranial Magnetic Stimulation
In transcranial magnetic stimuation (TMS) a magnetic coil placed over the scalp induces an electrical current in underlying brain regions. TMS can be applied to localized brain regions (focal areas) thought to be implicated in specific disorders. Manipulation of the magnetic field can stimulate an area of cortex as small as a quarter—

The primary clinical use of TMS, which the U.S. Food and Drug Administration formally approved in 2008, is for depression. Numerous studies report positive effects using TMS, but the required duration of treatment and the duration of beneficial effects remains under investigation.
The effects of brief pulses of TMS do not outlive the stimulation. Repetitive TMS (rTMS), however, which involves continuous stimulation for up to several minutes, produces longer-
In addition to treating depression, small but promising studies have extended the possible benefits of TMS to schizophrenic auditory hallucinations, anxiety disorders, neurodegenerative diseases, hemiparesis, and pain syndrome (Wassermann & Zimmerman, 2012).
Among the problems in all studies of TMS are questions related to the duration and intensity of stimulation and also to the area stimulated. Each person’s brain is slightly different, so to ensure that appropriate structures are stimulated, MRI must be performed on each subject.
Does TMS stimulation make the brain more plastic? If so, can learning be enhanced? The idea is, when a train of TMS is delivered, it produces a change in cortical excitability. This change in turn facilitates learning. Indeed, combined TMS and training can improve the therapeutic effects of motor or cognitive training given alone (Nevler & Ash, 2015).
Pharmacological Treatments
Several accidental discoveries, beginning in the 1950s, led to a pharmacological revolution in the treatment of behavioral disorders:
The development of phenothiazines (neuroleptics) to treat schizophrenia stemmed from a drug used to premedicate surgical patients. In the following decades, neuroleptic drugs became increasingly more selective, and they remain effective.
A new class of antianxiety drugs was invented: the anxiolytics. Medications such as Valium quickly became—
and remain— the most widely prescribed drugs in the United States. l-Dopa provided the first drug treatment for serious motor dysfunction in Parkinson disease. Once taken, l-dopa is converted into and replaces dopamine lost due to Parkinson disease.
The power of psychoactive drugs to change disordered behavior revolutionized the pharmaceutical industry. The central goal is developing drugs that can act as magic bullets to correct the chemical imbalances found in various disorders. Research is directed toward making drugs more selective in targeting specific disorders while producing fewer side effects. Both goals have proved difficult to achieve.
Pharmacological treatments have significant downsides. Acute and chronic side effects top the list, and long-
Section 6-2 classifies psychoactive drugs and their therapeutic effects.
Thus, although a medication may be useful for getting a person out of a depressed state, it may produce other symptoms that are themselves disturbing and may complicate recovery. Furthermore, in depression related to a person’s life events, a drug does not provide the behavioral tools needed to cope with an adverse situation. Some psychologists say, “A pill is not a skill.”
Negative side effects of drug treatments are evident in many people whose schizophrenia is being treated with neuroleptics. Antipsychotic drugs act on the mesolimbic dopamine system, which affects motivation, among other functions. The side effect emerges because the drugs also act on the nigrostriatal dopaminergic system, which controls movement. Patients who take neuroleptics also eventually develop motor disturbances. Tardive dyskinesia, an inability to stop the tongue, hands, or other body parts from moving, is a motor symptom of long-
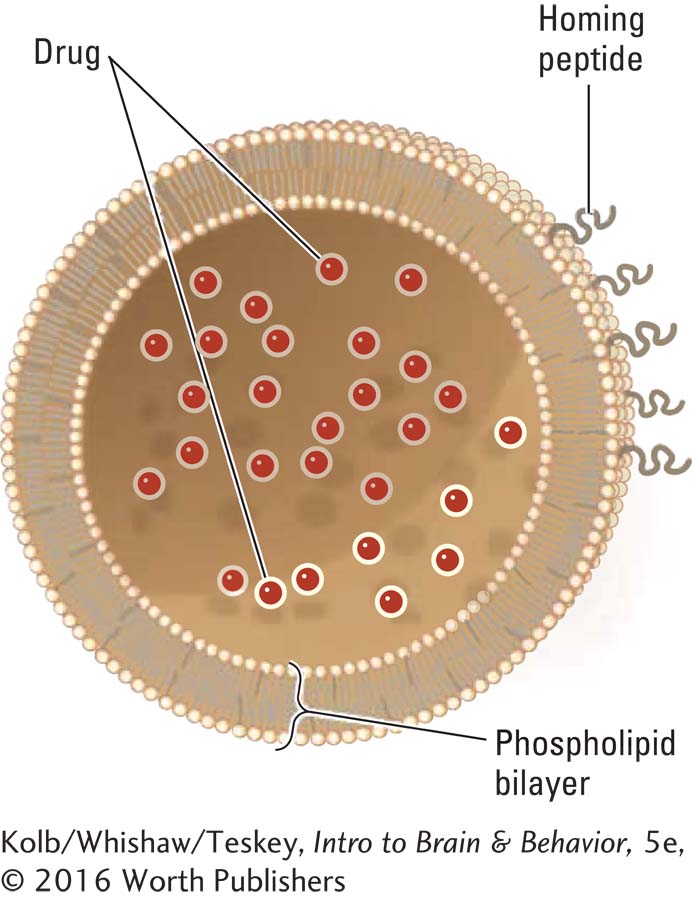
Despite their drawbacks, drugs do prove beneficial for many people. Improved drug chemistry will reduce side effects, as will improved delivery modes that bring a drug to a target system with minimal effects on other systems. One improved delivery system uses nanoparticles called liposomes, biosynthetic molecules 1 to 100 nm (nanometers, or billionths of a meter) in size. One natural biological nanoparticle, with a radius of about 40 nm, is the synaptic vesicle that houses a neurotransmitter for delivery into the cell’s extracellular space. Liposomes consisting of a synthetic vesicle with a homing peptide on the surface can, in principle, be constructed to carry a drug across the blood–
Behavioral Treatments
Treatments for behavioral disorders need not be direct biological or medical interventions. Just as the brain can alter behavior, behavior can alter the brain. Behavioral treatments focus on key environmental factors that influence how a person acts. As behavior changes in response to treatment, the brain is affected as well.
Focus 12-3 recounts a case of generalized anxiety disorder.
An example is treatment for generalized anxiety disorders attributed to chronic stress. People who endure a persistently high anxiety level often engage in maladaptive behaviors to reduce it. While they require immediate treatment with antianxiety medication, long-
Perhaps you are thinking that behavioral treatments may help somewhat in treating brain dysfunction, but the real solution must lie in altering brain activity. Since every aspect of behavior is the product of brain activity, behavioral treatments do act by changing brain function. If people can change how they think and feel about themselves or some aspect of their lives, this change has taken place because talking about their problems or resolving a problem alters how their brain functions. In a sense then, a behavioral treatment is a biological intervention. Behavioral treatments may sometimes be helped along by drug treatments that make the brain more receptive to change through behavioral therapy. In this way, drug treatments and behavioral treatments have synergistic effects, each helping the other to be more effective.
Your behavior is a product of all your learning and social experiences. An obvious approach to developing a treatment is to re-
BEHAVIOR MODIFICATION Behavioral therapies apply well-

COGNITIVE THERAPY Cognitive therapy operates from the perspective that thoughts intervene between events and emotions. Consider responses to losing a job. One thought could be, I’m a loser, life is hopeless. An alternative thought is, The job was a dead end. The boss did me a favor. The former cognition might lead to depression, whereas the latter would not. Cognitive therapies challenge a person’s self-
NEUROPSYCHOLOGICAL THERAPY If a relative or friend had a stroke and became aphasic, you would expect him or her to attend speech therapy—
Therapies for cognitive disorders resulting from brain trauma or dysfunction aim to retrain people in the fundamental cognitive processes they have lost. Although cognitive therapy seems as logical as speech therapy after a stroke, cognitive therapy assumes that we know what fundamental elements of cognitive activity are meaningful to the brain. Cognitive scientists are far from understanding these elements well enough to generate optimal therapies. Still, neuropsychologists are developing neurocognitive programs that can improve functional outcomes following TBI and stroke (Mateer & Sira, 2006; Sohlberg & Mateer, 1989). Treatment effectiveness can be improved with computer-
EMOTIONAL THERAPY In the 1920s, Sigmund Freud developed the idea that talking about emotional problems enables people to gain insights into the causes of the problems and serves as treatment too. Talk cures and other forms of psychological intervention may be broadly categorized as psychotherapies.
Since Freud’s time, many ideas have been put forth about the best type of therapy for emotional disorders. Key here is that for many disorders, whether neurological or psychiatric, medical treatments are not effective unless patients also receive psychotherapy. Indeed, the only effective treatment in many cases lies in addressing the unwanted behaviors directly—
Consider a 25-
For many people with emotional impairments resulting from brain disease or trauma, the most effective treatment for depression or anxiety is helping them adjust by encouraging them to talk about their difficulties. Group therapy provides such encouragement and is standard treatment in brain injury rehabilitation units.
PHYSICAL ACTIVITY AND MUSIC AS THERAPY Exercise and music have positive effects on peoples’ attitudes, emotional well-
REAL-
Focus 11-5 describes an effective low-
Think of rt-
VIRTUAL REALITY THERAPY The principle behind VR therapy is that patients enter or interact with a virtual world displayed on a computer screen or through goggles. One example is the Virtual Iraq and Afghanistan Simulation described in Research Focus 16-1. The participant can experience sights, sounds, even smells that mimic situations related to acquiring the behavioral disorder, in this case PTSD. In modified VR therapy a patient interacts as a character in a computer game. Winning the game necessitates making adaptive choices; maladaptive choices result in losing the game (Shin et al., 2015).
16-2 REVIEW
Classifying and Treating Brain and Behavioral Disorders
Before you continue, check your understanding.
Question 1
Three classifications of behavioral disorders are ____________, ____________, and ____________.
Question 2
____________ is the study of the distribution and causes of diseases in human populations.
Question 3
Developments in ____________ and ____________ have enabled their use in identifying brain and behavior disorders.
Question 4
Four treatment categories for behavioral disorders are ____________, ____________, ____________, and ____________.
Question 5
A therapy in which an electrode delivers stimulation directly to the brain is called ____________.
Question 6
An effective replacement for electroconvulsive therapy (ECT) is ____________.
Question 7
Why are classification systems useful even though they are inexact?
Answers appear in the Self Test section of the book.